Nummular eczema (nummular dermatitis, discoid eczema) is a distinct form of chronic eczema characterized by well-defined, coin-shaped patches with erythematous oozing and crusting. ICD-10 code: L30.0.
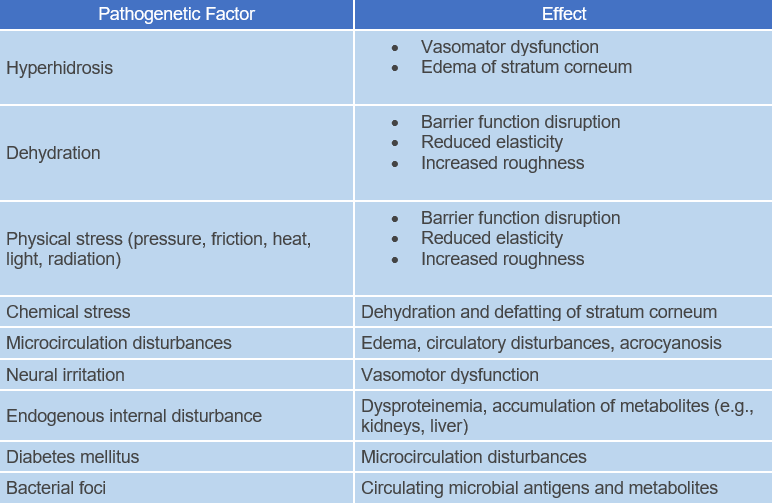
Nummular dermatitis is more common in men and typically presents between the ages of 40 and 70. The pathogenesis of the condition is not well understood; it may have a multifactorial etiology involving dysregulation of epidermal function. Such dysregulation could result from chronic vascular dystrophy (such as chronic venous insufficiency) or subtoxic cumulative exogenous irritation causing reversible physicochemical disruption of the skin's protective barrier function.
Microbial antigens may be another potential trigger for sensitization. Diseases of internal organs or infections (such as sinusitis, chronic tonsillitis, chronic bronchitis, bronchiectasis, chronic prostatitis, chronic dental infections) can sometimes serve as significant reservoirs of bacteria and trigger factors for the disease.
Contemporary microbial agents are not considered causative factors; however, the persistent and chronic nature of nummular dermatitis may result from contact allergy to microbial allergens. Recently, skin response to environmental aeroallergens has been discussed as an aspect of nummular dermatitis. Identification of the triggering factors is often challenging.
The eruptions typically appear on the distal parts of the limbs, especially the dorsal side of the hands, feet, forearms, and shins. In more severe cases, the shoulders and upper back may be affected. The disease begins with small, well-defined, coin-shaped areas of erythema that are slightly elevated above the skin surface and consist of papules and vesicles. After an acute exudative phase, the vesicles progress to an erosive stage. This leads to weeping, crusting and scaling. Individual eczematous patches may be 1-5 cm in diameter, but may coalesce into larger eruptions.
The condition may be localized, or numerous patches may spread rapidly. The differential diagnosis includes psoriasis and fungal infections. Patients experience severe pruritus. Response to treatment is typically poor, and the condition persists with exacerbations and remissions over months and years. The relapse rate is high. Mucous membranes are not involved.A thorough medical history helps identify triggering factors such as underlying diseases, infections, or medication use.
Bacteriological smears are necessary to detect infection.
Histological examination reveals psoriasiform epidermal thickening (acanthosis, hyper- or parakeratosis) with exudative inflammatory exocytosis and spongiosis. The upper dermal layer shows a perivascular lymphocytic infiltrate.
Search for underlying disease: Depending on the history, relevant investigations and laboratory tests are conducted to identify provocative factors.
Diagnostic tests to rule out major differential diagnoses:
- Microscopy of skin scrapings + KOH test to rule out tinea corporis.
- Patch test to rule out allergic contact dermatitis.
- Total serum IgE, atopy patch test to rule out atopic eczema.
- Tinea corporis
- Psoriasis
- Asteatotic eczema
- Large plaque parapsoriasis
- Impetigo
- Allergic contact dermatitis
General Treatment Recommendations
- It is necessary to eliminate triggering factors and address the underlying condition.
- Avoidance of skin-irritating contacts is essential. Anti-inflammatory and anti-eczema treatment (such as glucocorticoids, tar, dyes, antiseptics, and ultraviolet irradiation) should be adapted to the clinical presentation. In severe and extensive cases, systemic treatment with glucocorticoids (prednisone 0.5-1.0 mg/kg) and antibiotics is recommended.
- Systemic antihistamines are often needed to alleviate itching.
Recommended Treatment Approaches
- Topical glucocorticoids;
- Topical calcineurin inhibitors.
- Emollients;
- Tar preparations;
- Systemic glucocorticoids;
- Systemic antibiotics;
- UVB phototherapy
Treatment Based on Disease Stage
Acute Nummular Eczema
Characterized by vesicles, exudation, erosion, crusts
To prevent exacerbations during the acute exudative phase, fatty preparations should not be used. Initially, a glucocorticoid cream is applied in combination with moist dressings. After 2-3 days, when weeping, vesicles and ulceration have subsided and the area has epithelialized: Use topical corticosteroids twice daily for 1-2 weeks.
Topical calcineurin inhibitors may be used as an alternative to topical steroids. Topical calcineurin inhibitors begin to take effect 1-2 weeks after application. Read the contraindications (topical calcineurin inhibitors should not be used in the presence of a viral or bacterial superficial infection). In severe cases, oral glucocorticoids (e.g., prednisone 40 mg daily for 2 weeks with gradual dose reduction) are prescribed along with antibiotics (e.g., doxycycline or cephalosporin). Systemic antihistamines (e.g., dimethindene, hydroxyzine) relieve itching.
Subacute or Chronic Nummular Eczema
Characterized by:
- Erythema, edema, papules, scales
- Dry scaling, psoriasiform scaling, lichenification, infiltrated papules
- Hyperkeratotic patches
If the lesions are dry, less potent steroids (mometasone) on a non-greasy basis (lotion, cream) can be chosen, if necessary in combination with antiseptics. The steroid content should be gradually reduced and replaced by non-steroidal preparations. Tar mixtures (ichthammol 2-5%, liquor carbonis detergents 3-5%, thymol 3-10% based on lotion, zinc paste or cream) have good anti-eczema, antipruritic and antimicrobial properties.
Infiltrated and treatment-resistant lesions can be treated with intradermal injections of glucocorticoids (e.g., triamcinolone). Oil and oil-tar baths add to the therapeutic effect.
Topical calcineurin inhibitors may be used as an alternative to topical steroids. Topical calcineurin inhibitors begin to take effect 1-2 weeks after application. Read the contraindications (topical calcineurin inhibitors should not be used in the presence of viral or bacterial superficial infections).
Avoid dehydration of the skin caused by soaps, cleansers and improper care. The subacute stage of nummular eczema is an appropriate time to begin UV therapy. Be aware of the phototoxic effects of tar preparations.
Alternative Treatment Methods
PUVA Phototherapy: UVA irradiation (320-400 nm) is administered 2 hours after oral intake of the photosensitizing psoralen, 8-methoxypsoralen (0.6-0.8 mg/kg). Treatment begins with a dose of 0.5-1.0 J/cm2, which is then individually adjusted according to the patient's sensitivity. Treatment sessions are performed 3-4 times per week for 3-4 weeks.
While taking psoralen, UVA protective goggles must be worn for 24 hours to prevent premature cataract formation. Male genitals should be covered with foil.
Possible side effects include sunburn, premature skin aging, increased risk of basal cell and squamous cell carcinoma, nausea, and liver function abnormalities. Rarely, blistering, pain, and development of erythroderma may occur. According to published results, there is no clear difference between SUP and PUVA. The duration of treatment is shorter with PUVA therapy. UV therapy for nummular eczema results in longer remission periods after discontinuation of systemic or topical steroids, with a reduced risk of relapse.
The immunosuppressive drug cyclosporine A has been used with some success in several dermatologic conditions, including atopic eczema and psoriasis. However, its use is limited by systemic side effects. Attempts to use topical forms of the drug have been made, but without success.