Herpes zoster, also known as shingles, is a viral disease of the skin and nervous tissue caused by reactivation of herpes simplex virus type 3 (varicella-zoster virus, VZV). It is characterized by the appearance of predominantly blistering rashes on a background of erythema in a specific dermatomal area affecting the posterior roots of the spinal cord and ganglia of peripheral nerves. ICD-10 Code: B02.
The incidence of herpes zoster varies in different countries around the world, ranging from 0.4 to 1.6 cases per 1000 people per year in individuals of different age groups:
- 1.1-2.9 per 1000 people under 50 years old.
- 4.6-6.9 per 1000 people for ages 50-59 and 60-69.
- 9.5-10.9 per 1000 people for ages 70-79 and 80 and older.
The causative agent of the disease is the varicella-zoster virus (VZV), a member of the Alphaherpesviridae subfamily of the Herpesviridae family. It is a nucleotide 30-50 nm in diameter enclosed in one or more oval membranes. There is only one serotype of herpes zoster virus. Primary infection with varicella-zoster virus typically manifests as chickenpox.
Infection with virus occurs by airborne transmission, followed by replication in the mucous membranes of the respiratory tract. People who have had chickenpox usually develop lifelong immunity to it. However, when this immunity weakens, especially in adults, reactivation of the virus can lead to shingles. During the course of the disease, VZV invades the sensory nerve endings from the skin and mucous membrane lesions, travels along their fibers to the sensory ganglia, and ensures its persistence in the human body. The virus most often persists in the first branch of the trigeminal nerve and spinal ganglia from T1 to L2.
The risk of developing the disease in immunocompromised patients is more than 20 times higher than in people of the same age with normal immunity. Immunocompromised conditions associated with a high risk of developing shingles include HIV infection, bone marrow transplantation, leukemia, lymphoma, chemotherapy, and treatment with systemic glucocorticosteroids. Shingles may also be an early marker of HIV infection, indicating the first signs of immunodeficiency.
In uncomplicated cases, the virus can be isolated from exudative lesions up to seven days after the onset of the rash (this period is prolonged in immunocompromised patients). In uncomplicated forms, the virus is spread by direct contact with the rashes, while in disseminated forms the infection can be transmitted by airborne droplets.
Classification:
- B02.0 Zoster encephalitis
- B02.1 Zoster meningitis
- B02.2 Zoster with other nervous system involvement
- Postherpetic:
- Ganglionitis of the geniculate ganglion of the facial nerve
- Polyneuropathy
- Trigeminal neuralgia
- Postherpetic:
- B02.3 Zoster ocular disease
- Blepharitis
- Conjunctivitis
- Iridocyclitis
- Iritis
- Keratitis
- Keratoconjunctivitis
- Scleritis
- B02.7 Disseminated zoster
- B02.8 Zoster with other complications
- B02.9 Zoster without complications
Prodromal period:
During this period, pain and paresthesia (tingling or numbness) (less commonly, itching, tingling, or burning) occur in the area affected by the dermatome. The pain may be intermittent or constant and may be accompanied by hyperesthesia of the skin. The pain syndrome may mimic pleuritis, myocardial infarction, duodenal ulcer, cholecystitis, renal or hepatic colic, appendicitis, intervertebral disc prolapse, early-stage glaucoma, leading to diagnostic and treatment challenges. Pain during the prodromal period may be absent in patients under 30 years of age with normal immune system.
Stages of rash development in herpes zoster:
Erythematous-Papular Stage
Vesicular stage
Regression stage
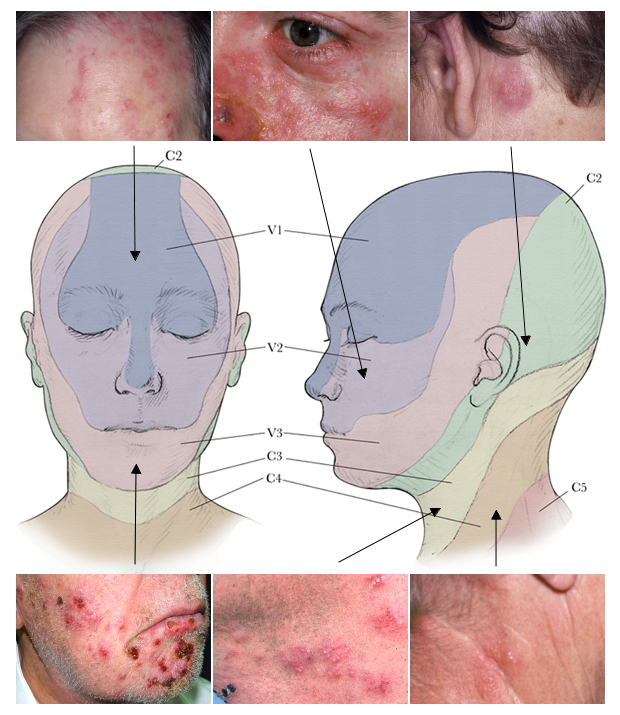
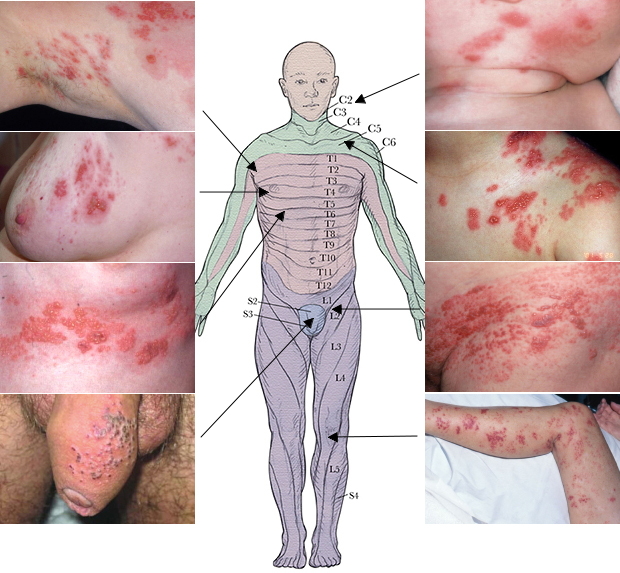
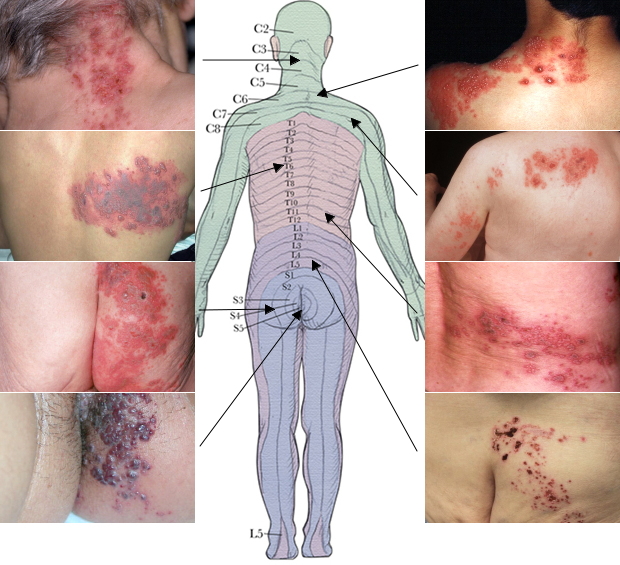
Localization of Herpes Zoster by Dermatomes
A characteristic feature of lesions in herpes zoster is their location and distribution, which are observed unilaterally and limited to the area innervated by a single sensory ganglion.
Areas of trigeminal nerve innervation, especially the ophthalmic branch, are most commonly affected by herpes zoster, as well as the skin of the T3-L2 segments of the trunk. Skin lesions on the chest are observed in more than 50% of cases, and rashes are least likely to occur on the skin of the distal extremities. The lesions may be located in the sacral region, leading to the development of a neurogenic bladder picture with urinary dysfunction and retention (due to virus migration to adjacent autonomic nerves); it may be associated with herpes zoster of the sacral dermatomes S2, S3, or S4.
Common symptoms
The clinical picture of herpes zoster includes both cutaneous manifestations and neurological disorders. Approximately 20% of patients experience general symptoms such as fever, headache, malaise, increased fatigue, regional lymph node enlargement, and cerebrospinal fluid changes (lymphocytosis and monocytosis). Pain often precedes skin changes and, with appropriate localization, may mimic myocardial infarction, appendicitis, renal colic, etc. The most common site of pain is along the intercostal nerves.
Abortive herpes zoster (incognito)
Bullous herpes zoster
Hemorrhagic herpes zoster
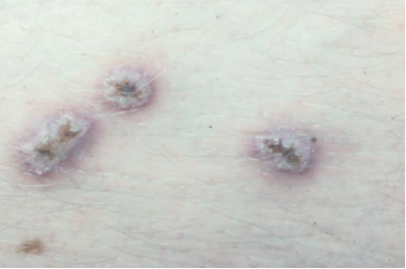
Gangrenous herpes zoster
Generalized Herpes Zoster
In some patients (2-4%), a generalized form of herpes zoster is observed: in addition to the usual site of infection, a more or less widespread rash consisting of vesicles, resembling elements of chickenpox, appears throughout the entire skin along with eruptions along the nerve trunk. Recurrent episodes of infection in the form of generalized rashes are usually not observed.
In the presence of immunodeficiency (including HIV infection), skin manifestations can appear far from the affected dermatome, known as the disseminated form. The likelihood and degree of dissemination of lesions on the skin increase with the patient's age. Disseminated forms include:
- Herpes zoster with acute disseminated skin lesions: Multiple vesicles and blisters on different areas of the skin and mucous membranes. After the vesicles and blisters rupture, erosions form, which then dry and form scabs. The number of elements varies from two or three to several hundred. The clinical picture resembles a combination of chickenpox and herpes zoster.
- Herpes zoster with chronic disseminated skin lesions: Vesicles and blisters (including on the palms and soles) appear continuously. They may be generalized or limited to one or more dermatomes. Vesicles and blisters leave behind nodules, ulcers and ecthyma-like elements (deep ulcers covered with scabs). Healing is prolonged and post-inflammatory hypo- or hyperpigmentation may occur.
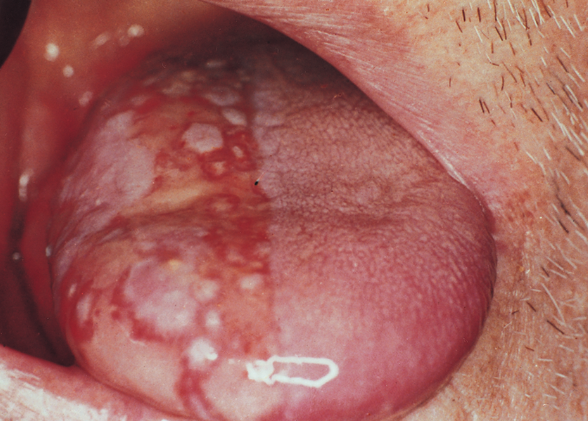
Oral Herpes Zoster
Hyperkeratotic herpes zoster
Herpes zoster ophthalmicus
Herpes zoster ophthalmicus is the herpetic involvement of any branch of the ophthalmic nerve. In 10-15% of patients, the ophthalmic branch of the trigeminal nerve may be involved, with eruptions on the skin extending from the level of the eye to the temporal region, with a sharp termination along the midline of the forehead. Involvement of the nasociliary branch, which innervates the eye, tip and lateral parts of the nose, allows the virus to invade the ocular structures. The cornea is often involved, leading to the development of keratitis. In addition, other parts of the eyeball may be affected, resulting in episcleritis, iridocyclitis, and inflammation of the iris.
The retina is rarely involved in the pathological process (as hemorrhages or emboli), but the optic nerve is more often affected, leading to optic neuritis with subsequent atrophy (possibly due to the extension of meningeal processes to the optic nerve). In herpes zoster with ocular involvement, the eruptions spread from eye level to the top of the head, but do not cross the midline.Hunt syndrome
Hunt syndrome is a ganglionitis of the geniculate ganglion of the facial nerve caused by the varicella-zoster virus. It manifests as pain in the ganglion, often radiating to the face, occiput, neck, eruptions in the external auditory canal, tympanic membrane, sometimes on the tongue and palate, paralysis of the facial muscles, and vestibulocochlear nerve involvement with dizziness, tinnitus, and hearing loss on the affected side.
Characteristics of Hunt syndrome include pain in the external auditory canal, eruptions in the external auditory canal, facial muscle paralysis, and decreased taste sensation in the anterior two-thirds of the tongue.Herpes Zoster in Children
Intrauterine infection is possible in newborns whose mothers had a primary infection with varicella-zoster virus (VZV) during pregnancy. These children develop herpes zoster without prior chickenpox. Infantile herpes zoster often results in temporary paralysis of the affected limb.
There have been rare reports of herpes zoster in young children. Risk factors for occurrence in children include maternal chickenpox during pregnancy or primary VZV infection in the first year of life. The risk of developing the disease is higher in children who have had chickenpox before the age of 1 year. Herpes zoster in children is generally less severe than in older patients, with milder pain symptoms, and postherpetic neuralgia is less common.Herpes zoster in HIV-infected patients
The risk of developing herpes zoster is higher in HIV-infected patients, and recurrences of the disease are more common. Additional symptoms may occur due to motor nerve involvement (in 5-15% of cases). The course of herpes zoster is more prolonged in HIV-infected individuals, and gangrenous and disseminated forms occur more frequently (25-50%), with severe internal organ (lung, liver, brain) involvement noted in 10% of cases in this category. In HIV-infected individuals, recurrences of herpes zoster involving one or more adjacent dermatomes are common.
Herpes zoster in pregnant women
The disease in pregnant women may be complicated by the development of pneumonia or encephalitis. VZV infection in the first trimester of pregnancy leads to primary placental insufficiency and is usually associated with pregnancy loss. The presence of infection should be the basis for intensive prevention of hemodynamic consequences (placental insufficiency, intrauterine hypoxia, intrauterine fetal growth restriction).
Pain syndrome in herpes zoster:
Pain is the primary symptom of herpes zoster. It often precedes the development of the rash and may persist after the rash has resolved, leading to postherpetic neuralgia. Pain in herpes zoster and postherpetic neuralgia is caused by different mechanisms. In the early stages, anatomical and functional changes occur that lead to the development of neuralgia - this explains the relationship between the severity of the initial pain and the subsequent development of postherpetic neuralgia, as well as the reasons for the failure of antiviral therapy in its prevention.
Pain syndrome associated with herpes zoster has three phases: acute, subacute, and chronic (postherpetic neuralgia). The acute phase of pain occurs during the prodromal period and lasts up to 30 days. The subacute phase of pain follows the acute phase and lasts no longer than 120 days. Pain lasting longer than 120 days is defined as postherpetic neuralgia, which can persist for several months or years, causing physical suffering and significantly reducing the quality of life of patients.
The immediate causes of prodromal pain are subclinical reactivation and replication of VZV in nerve tissue. Damage to peripheral nerves and neurons in ganglia serves as a trigger for afferent pain signals. In some patients, the pain syndrome is accompanied by generalized systemic inflammatory manifestations such as fever, malaise, myalgia, and headache.
In the majority of immunocompetent patients (60-90%), severe acute pain is accompanied by the appearance of a skin rash. The significant release of excitatory amino acids and neuropeptides caused by the blockade of afferent impulses during the prodromal and acute stages of herpes zoster can lead to toxic damage and death of inhibitory interneurons in the posterior horns of the spinal cord. The severity of acute pain increases with age. Excessive nociceptor activity and the generation of ectopic impulses can lead to increased and prolonged central responses to normal stimuli, known as allodynia (pain and/or unpleasant sensations induced by stimuli that are not typically painful, such as clothing touching the skin).
Predisposing factors for the development of postherpetic neuralgia include age over 50 years, female gender, the presence of prodromal symptoms, extensive rash, rash localization within the area of innervation of the trigeminal nerve or brachial plexus, severe acute pain, and immunodeficiency.
Three types of pain can be distinguished in postherpetic neuralgia:
- Constant, deep, dull, pressing, or burning pain.
- Spontaneous, periodic, stabbing, shooting, similar to an electric shock.
- Allodynia.
Pain syndrome is typically accompanied by sleep disturbances, loss of appetite and weight, chronic fatigue, depression, leading to social maladaptation of patients.
The diagnosis of herpes zoster is based on:
- Typical complaints (manifestations of neurological symptoms).
- The course of the disease (prodromal period and skin manifestations).
- Clinical features on the skin (the combination of painful sensations along the nerve pathway with linearly arranged groups of blisters on the skin within one or more dermatomes).
When necessary for diagnosis verification, laboratory tests are used:
- PCR to identify the Varicella zoster virus present in material from lesions on the skin and/or mucous membranes.
- Tzanck smear (Tzanck test) allows for the rapid identification of characteristic multinucleated epithelial cells but does not differentiate between the herpes simplex virus and the varicella-zoster virus. Therefore, direct immunofluorescence (DIF) is preferable.
- Viral culture is not a highly sensitive test, and it may take up to 7 days to obtain results.
- Herpes simplex
- Dermatitis Herpetiformis
- Bullous Pemphigoid
- Pemphigus Herpetiformis
- Allergic Contact Dermatitis
- Eczema herpeticum
- Impetigo
- Eczema
- Chickenpox(varicella)
Treatment Goals:
- Resolution of clinical symptoms of the disease.
- Prevention of complications.
General Remarks on Therapy
- The presence of peripheral ganglion and nerve tissue lesions, as well as ocular involvement in herpes zoster, requires the involvement of specialists with the appropriate profile: treatment of postherpetic neuralgia and ophthalmic herpes should be performed with neurologists and ophthalmologists.
- Antiviral drugs are necessary for the effective control of VZV infection.
- In cases of severe pain syndrome, analgesic medications are prescribed.
- The aim of topical treatment is to speed up the regression of the skin rash, to reduce the signs of inflammation and to prevent a bacterial super-infection. The necessity of anti-inflammatory treatment depends on the development of herpetic neuralgias associated with pain syndrome, and if indicated, it should be individually tailored.
- Avoid the use of occlusive dressings.
- Topical treatment with antiviral and analgesic agents is not effective.
Antiviral Therapy
Prescribing antiviral drugs is most effective within the first 72 hours of clinical symptoms of the disease:
- Acyclovir 800 mg orally 5 times a day for 7 days, or
- Famciclovir 500 mg orally 3 times a day for 7 days, or
- Valacyclovir 1000 mg orally 3 times a day for 7 days.
The reduced sensitivity of VZV to acyclovir and the high level of antiviral activity determine the preference for prescribing famciclovir or valacyclovir for treatment.
Anti-inflammatory therapy
Nonsteroidal anti-inflammatory drugs may be prescribed.
In the absence of analgesic effect, drugs with central analgesic action and neural blocks (sympathetic and epidural) may be used, as determined in consultation with a neurologist.
Systemic Corticosteroids:
Orally administered corticosteroids are commonly used in the treatment of herpes zoster, even though clinical trials have shown variable results. Prednisone used in conjunction with acyclovir has been shown to reduce the pain associated with herpes zoster.
- Prednisone 25 mg/day orally for two weeks
Systemic Interferons:
- Interferon-gamma 500,000 IU once daily subcutaneously every other day, for a course of 5 injections.
Treatment for Children
- Acyclovir 20 mg per kg orally 4 times a day for 5 days.