Herpes labialis is an infectious disease caused by the herpes simplex virus that localizes on the face, lips, and oral mucosa (including the palate, tongue, back of the throat, and gums). ICD-10 Code: B00.1, B00.2
The prevalence of herpes simplex virus type 1 (HSV-1) is high in all regions of the world. In the 1950s, 90% of the population over 30 years old had serological evidence of HSV-1 infection. In recent years, this rate has decreased to 60-80% in some Western countries, due to improved hygiene.
Infection has two peaks: the first occurs between 6 months and 3 years of age, and the second occurs after sexual maturity due to oral-oral or oral-genital transmission of the infection. Most cases of orofacial HSV infection are caused by HSV-1, but in some cases infections caused by HSV-2 have been reported in sexually active individuals and HIV-positive patients.
Herpes simplex viruses are transmitted from person to person by direct contact with infected lesions on the skin, mucous membranes, and with secretions.
The success of HSV as a pathogen and the key to its survival is the ability of the virus to remain in a latent form in sensory ganglia (trigeminal ganglia in the case of Herpes labialis) throughout the life of the host organism. The virus enters nerve cells and binds to them immediately after axonal contact, and nucleocapsids enter the neuronal nucleus by retrograde axonal transport.
There are two types of orofacial herpes:
- Primary (occurs as a result of the first contact with the virus)
- Recurrent.
Primary infection
In most cases, primary infections are asymptomatic and clinical manifestations are observed in a minority of infected individuals. After an incubation period (2-14 days), the disease presents as herpetic gingivostomatitis or dermatitis.
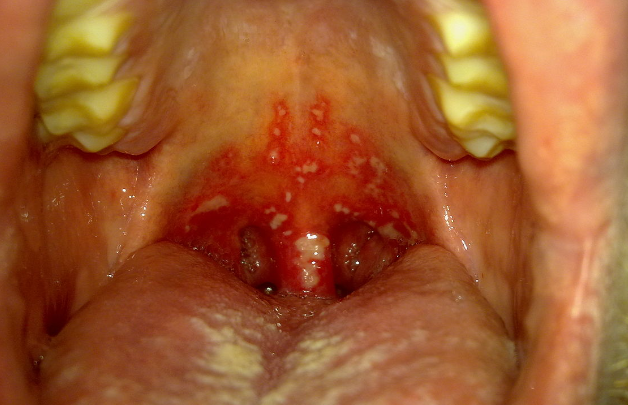
Herpetic Gingivostomatitis
Herpes labialis
Typical location for outbreaks is around the mouth, especially the red border of the lips and nose. In rarer cases, the rash may appear on the cheeks, temples, eyelids, or earlobes; this localization is known as herpes gladiatorum because it is often seen in wrestlers. The eruptions consist of clustered, semi-spherical vesicles on an erythematous and swollen base. Patients may experience burning, tingling, and itching in the areas where the rash will later appear. After the vesicles rupture, erosions and crusts form.
Skin lesions usually resolve within 10-14 days. In cases of secondary infection, recurrences may persist for 3-4 weeks.Atypical Forms of Herpes labialis:
- Zosteriform herpes simplex is characterized by the appearance of vesicles along the course of specific nerves on the face, limbs, or buttocks. It differs from shingles (herpes zoster) in that there is no severe pain radiating along the nerves.
- Abortive herpes simplex occurs on areas of the skin with thickened epidermis, such as the palms and fingertips. It presents as barely noticeable vesiculo-papular elements accompanied by itching, burning, and nerve pain.
- Edematous herpes simplex occurs in areas with loose subcutaneous tissue, such as the eyelids and lips. Severe edema obscures the primary elements.
- Elephantiasis-like herpes simplex is an edematous form that leads to persistent lymphedema in the affected area.
- Ulcerative herpes simplex is characterized by the development of small ulcers at the sites of typical herpetic eruptions. These ulcers grow slowly and do not epithelialize over time. If they persist for more than 3 months, they are considered to be AIDS-related.
- Hemorrhagic herpes simplex presents with vesicles containing bloody fluid and can occur anywhere on the skin.
- Hemorrhagic-necrotic herpes simplex is characterized by necrosis at the site of eruptions and scarring.
Complications of Primary Infection
Common complications of primary infection include:
- Eczema herpeticum in atopic patients.
- Keratoconjunctivitis.
- Autoinoculation.
- Dissemination of HSV infection in other skin conditions, such as Darier's disease, mycosis fungoides, ichthyosis vulgaris, and congenital ichthyosiform erythroderma.
Recurrent Infection
Based on the natural history of HSV-1, the infection is now defined as a persistent chronic infection of sensory ganglia with varying degrees of epithelial expression. Up to 40% of individuals infected with HSV-1 will experience clinical recurrence at some point. As for asymptomatic shedding of HSV-1 in saliva, it has been reported in 1-10% of cases in adult patients.
Factors that can trigger virus reactivation include:
- Exposure to sunlight
- Illness with fever.
- Stress.
- Premenstrual tension.
- Surgeries
- Dental surgical procedures.
- Dermabrasion, including laser therapy.
Most people who experience a recurrent infection have a prodromal phase with sensations of burning, itching, numbness, and/or pain. This phase lasts 6-12 hours and is followed by clinical symptoms. Groups of vesicles appear on an erythematous or papular base at the junction of the skin and mucous membranes of the lips and internal keratinized areas of the oral cavity, such as the gums and hard palate. The ulceration phase is very short, followed by a long crust formation phase with an average duration of 130 hours. The total healing time is 7-10 days.
The diagnosis is based on history and specific tests:
- PCR to identify the virus present in material from lesions on the skin and/or mucous membranes.
- Tzanck smear (Tzanck test) allows for the rapid identification of characteristic multinucleated epithelial cells but does not differentiate between the herpes simplex virus and herpes virus. Therefore, direct immunofluorescence (DIF) is preferable.
- Viral culture is not a highly sensitive test, and it may take up to 7 days to obtain results.
- Aphthous Stomatitis
- Herpes Zoster
- Allergic Contact Dermatitis
- Contact Stomatitis
- Herpetic tonsillitis
- Erythema Multiforme
- Bullous Impetigo
- Hand, Foot, and Mouth Disease
- Chemotherapy-Associated Stomatitis
- Stevens-Johnson Syndrome / Toxic Epidermal Necrolysis
- Pemphigus vulgaris
- Acute Necrotizing Ulcerative Gingivitis
General Remarks on Therapy
- Oral or intravenous antiviral drugs can be used to treat primary infections with clinical symptoms in seronegative children and adults.
- It is important to educate patients to avoid oral-oral and oral-genital contacts when clinical manifestations of herpes are present. The prevalence of genital herpes caused by HSV-1 is increasing in Europe.
- Sunscreens may help prevent relapses in patients who experience recurrences triggered by ultraviolet radiation.
- Patients with frequent and severe relapses may be prescribed suppressive antiviral medications.
- Immunocompromised patients and atopic individuals should receive systemic treatment. The dosage may be higher and the duration of treatment may be longer.
- Recurrent erythema multiforme associated with HSV can be alleviated by prescribing suppressive antiviral drugs.
Recommended Treatment Methods
Primary Infection
- Acyclovir orally 15 mg/kg 5 times a day for 7 days (children).
- Acyclovir 400 mg orally 5 times a day for 7 days, or
- Famciclovir 200 mg orally 3 times a day for 7 days, or
- Valacyclovir 500 mg orally 2 times a day for 7 days.
Episodic Treatment of Recurrent Disease
Topical Episodic Treatment
- Docosanol 10% 5 times a day for 5 days
Systemic Episodic Treatment
- Acyclovir orally 200 mg 5 times a day for 5 days.
- Valacyclovir orally 2g twice a day for 1 day. The second dose should be taken approximately 12 hours (but no sooner than 6 hours) after the first dose.
- Famciclovir orally 1500 mg once a day for 1 day or 750 mg twice a day for 1 day.
Suppressive Treatment
Use of antiviral drugs can reduce the frequency of relapses during treatment by 50-78%. Duration of the treatment is 6-12 months.
- Acyclovir orally 400 mg twice a day.
- Valacyclovir orally 500 mg once a day.
- Famciclovir orally 250 mg twice a day.
Suppressive treatment is recommended for:
- Patients with frequent relapses (>6 episodes per year).
- Patients with severe and prolonged episodes (including atopic patients).
- Patients with severe episodes associated with ultraviolet radiation.
- Herpes simplex in association with recurrent erythema multiforme.
- Patients undergoing chemical or abrasive procedures on the face for cosmetic purposes.
Sun Protection
Two randomized double-blind crossover studies have demonstrated a significant reduction in recurrence severity when using sunscreen products.