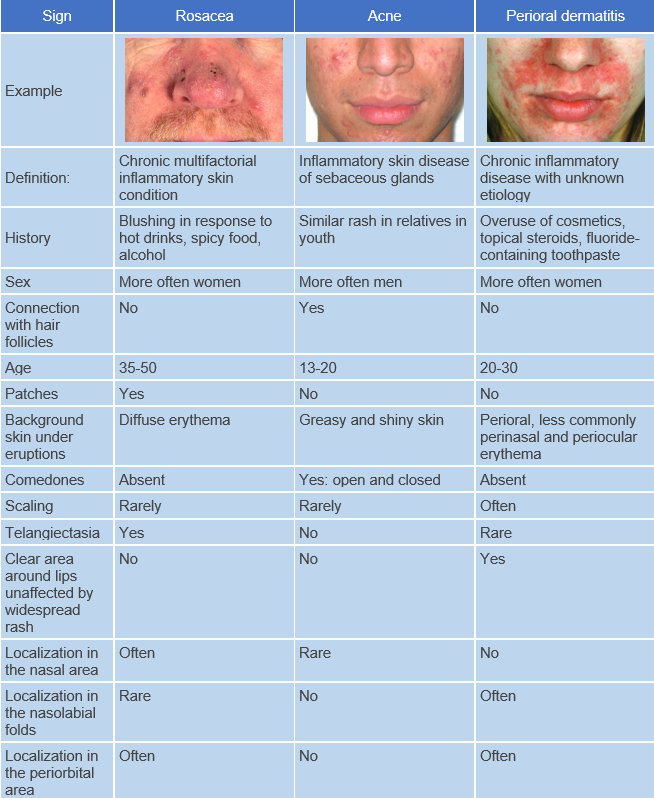
Perioral dermatitis is a chronic recurrent skin disease characterized by erythematous-papular, papulovesicular, and less commonly papulopustular eruptions, primarily in the perioral area. ICD-10 Code: L71.0
The prevalence of perioral dermatitis among the population is approximately 0.5-1%, predominantly affecting women aged 15-45 years. Perioral dermatitis may also occur in children, with a peak incidence during puberty, and is more commonly observed in boys. Approximately 2% of patients who visit a dermatologist have perioral dermatitis. People with fair skin are more likely to be affected.<-p>
The following factors may contribute to the development of perioral dermatitis:<-p>
- Prolonged use of glucocorticosteroids (topical or systemic).
- Demodex mites.
- Infectious such as yeast-like fungi and some anaerobic bacteria.
- Use of cosmetic products (moisturizers, cleansers, sunscreens).
- Use of fluoride toothpaste.
- Ultraviolet radiation.
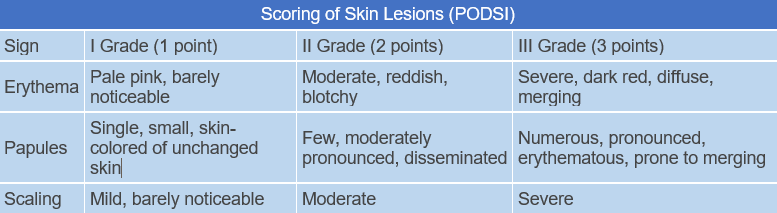
Depending on the severity of the clinical manifestations, perioral dermatitis is classified into mild, moderate, and severe forms. Granulomatous perioral dermatitis falls under the category of severe perioral dermatitis. An index called POdSI has been developed to determine the severity of perioral dermatitis based on the assessment of the degree of clinical manifestations such as erythema, papules, and scaling. The POdSI index value is the sum of the scores for the severity of erythema, papules and scaling according to the characteristics of the eruptions for each severity level. Here, "0" indicates the absence of the feature, 1, 2, 3 points indicate the severity of the feature, and intermediate levels of 0.5, 1.5, and 2.5 can also be used.
Mild perioral dermatitis corresponds to POdSI values of 0.5-2.5, moderate severity corresponds to 3.0-5.5, and severe POdSI ranges from 6.0 to 9.0.
The condition is characterized by erythema of varying severity with distinct borders, as well as semi-spherical non-follicular pinkish-red papules, papulovesicles, and less commonly, papulopustules measuring 1-2 mm in diameter. These eruptions are localized in the perioral and periorbital areas, in the nasolabial folds, and can also spread to the skin under the chin and cheeks. A characteristic feature of perioral dermatitis is the presence of unaffected pale skin around vermilion border.
Typical complaints from patients with perioral dermatitis include sensations of burning, tenderness, as well as tightness and tension of the skin in the affected area. Itching is possible but not characteristic.
Granulomatous Perioral Dermatitis
General Treatment Recommendations
The choice of medication and method of treatment for perioral dermatitis depends on the severity and stage of the disease. During the treatment period, regardless of the treatment method chosen, the use of cleansing and moisturizing cosmetics, decorative cosmetics, fluoridated toothpaste, topical and systemic medications containing glucocorticosteroids should be discontinued
Three types of treatment are distinguished: "zero," topical, and systemic therapy for perioral dermatitis. In cases of mild form, "zero" therapy may be sufficient, which involves discontinuing all topical, including cosmetic, products, especially those containing glucocorticosteroids. Improvement usually occurs within an average of 2 weeks.
Topical treatment
Prescribed for mild and moderate cases, it may be used as a monotherapy and in severe cases of perioral dermatitis it may be prescribed in combination with systemic treatment:
- Metronidazole, 1% cream, applied twice daily for 8 weeks.
- Azelaic acid, 20% cream, applied twice daily for 2 to 6 weeks.
- Pimecrolimus, 1% cream, applied twice daily for 4 weeks.
Systemic Therapy:
Prescribed for severe forms and in cases where topical treatment is ineffective:
- Doxycycline 100 mg twice a day or once a day for an 8-12 week
- Minocycline 100 mg twice a day or once a day, for an 8-12 week
- Tetracycline, 250–500 mg orally twice daily for 4–8 weeks. Administered to patients over 8 years old.
- In cases of tetracycline intolerance, in children under 8 years old, and in cases of granulomatous perioral dermatitis in children: erythromycin, 250 mg orally twice daily for 1–4 months.
In cases where antibacterial therapy is ineffective, isotretinoin is prescribed at a dosage of 0.1-0.7 mg per kg of body weight orally once daily for 6-20 weeks.