Lichen simplex chronicus (LSC) is an acquired, pruritic, chronic dermatosis characterized by localized lichenified plaques that result from repeated rubbing and scratching of normal skin. ICD-code - L28.0.
There is no known predisposing skin condition or clear cause for the development of lichenification. However, it may develop secondary to a chronic eczematous process. Differences in clinical morphology, size, and location of the lesions have led to the classification of the disease into several clinical forms that are prevalent worldwide. It is particularly common in individuals of Asian descent and relatively rare in black populations. LSC predominantly affects women, with the peak incidence occurring between the ages of 30 and 50. Itching is believed to be not only a symptom but also a major cause of the disease. It is the primary factor leading to lichenification, probably due to the activity of mediators or proteolytic enzymes. Emotional stress and psychovegetative disorders can lead to an unconscious habit of rubbing and constant scratching of the skin, resulting in skin thickening and accentuated skin wrinkles.
Lichenification may also be secondary to many pruritic dermatoses, and some authors suggest that lichen simplex chronicus is a minimal variant of atopic eczema in adults with a personal or family history of atopic disorders. Others believe that the development of the disease is associated with internal organ dysfunction, such as gallbladder pathology, diabetes, and constipation. Lichenification may also develop in other irritant dermatoses or as a complication of persistent skin lesions of various types, such as chronic contact dermatitis, stasis dermatitis, seborrheic dermatitis, flat lichen, anal and vulvar pruritus, and, rarely, psoriasis.
The distinction between lichenification and some forms of prurigo is not entirely clear in terminology and practice. In some patients, chronic rubbing and scratching may lead to the formation of nodules known as nodular prurigo or nodular lichenification. Increased levels of neuropeptides, calcitonin gene-related peptide, and substance P in nerve fibers may be associated with severe pruritus. Some patients, such as blacks, may develop papular and follicular lichenification. There may be an innate predisposition to the development and persistence of lichenification.Severe, paroxysmal pruritus typically occurs, often at night, and is often disproportionate to the extent of objective skin changes.
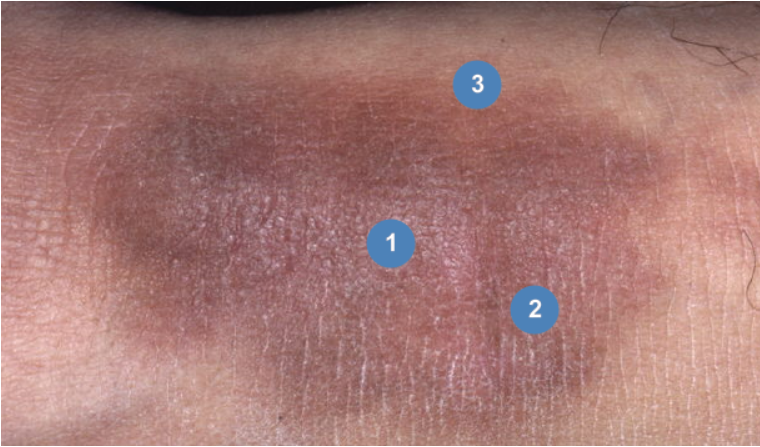
The initial lesion is usually isolated and its structure can be divided into three zones:
- Central zone with infiltration and primary lichenification.
- Middle zone with closely spaced lichenoid papules.
- Peripheral zone with slight thickening and pigmentation.
Lichen simplex chronicus. Neck area.
The diagnosis of lichen simplex chronicus is based on the clinical presentation and biopsy.
- Atopic eczema
- Nummular eczema
- Psoriasis
- Chronic eczema
- Hypertrophic lichen planus
- Lichen amyloidosis
- Nodular prurigo
- Tinea corporis
- Drug eruptions
- Cutaneous T-cell lymphoma
- Stasis dermatitis
General Therapeutic Recommendations
- Treatment should be individualized for each patient depending on various precipitating factors, localization and duration of specific lesions.
- Lesions worsen during periods of fatigue and emotional stress and improve with rest and relaxation.
- In most cases, rubbing and scratching is a reflex, unconscious habit. Explaining to the patient the mechanism of the "itch-scratch" cycle and its relationship to the disease may help to overcome this habit.
- Some patients may require psychiatric consultation, and psychotherapy may be recommended. These are usually individuals who are experiencing emotional distress or functional complaints.
- Searching for the underlying disease associated with lichenification is essential.
- During active treatment, patients should avoid the use of soap and detergents when washing the affected areas and should keep their nails short.
Systemic Therapy
Itching is the leading symptom of the disease, and treatment should aim to alleviate itching.
- Antihistamines are widely used, and the most useful route of administration is usually oral or parenteral. Hydroxyzine hydrochloride, diphenhydramine hydrochloride, chlorpheniramine and promethazine are known as classical antihistamines that block H1 receptors. These drugs are recommended to control itching. Cetirizine, loratadine, and mizolastine are second-generation antihistamines that are preferred for itch control in socially active patients because these drugs do not have a sedative effect. Cyproheptadine hydrochloride is another effective drug for itch control.
- Antidepressants and anxiolytics: In many cases, antihistamines are not effective enough and may be replaced with psychotropic medications. Tranquilizers suppress the urge to scratch and reduce nervous tension. Tricyclic antidepressants may be an alternative to control itching as they effectively bind to H1. Amitriptyline may be prescribed to patients with neuroses and depression to prevent the tendency to scratch.
- Antibiotics: In cases of complications with secondary infection, appropriate antibiotics must be prescribed. The primary pathogen in these patients is Staphylococcus aureus.
Topical Treatment
- Corticosteroids: High-potency corticosteroids help relieve pruritus and reduce lesion infiltration. In both cases, the use of very potent topical steroids and steroids under occlusion is recommended for a short period of time. If the lesion is in the genital area, it is preferable to use low-potency steroids.
- Tar: Anti-inflammatory properties of tar and its products are well known. Pure coal tar can be prescribed for several days. It is best to use it with emollients, as tar can dry out the skin. Side effects may include photosensitization, contact dermatitis, and folliculitis. Combined therapy is well tolerated, including steroids and tar with or without aspirin.
- Urea: Urea-containing products have been successfully used in the treatment, maintenance and prevention of neurodermatitis. Their efficacy is based on their ability to increase the water-binding capacity of the stratum corneum as well as their keratolytic, antipruritic and antiproliferative effects. Combined use of urea and hydrocortisone can be beneficial in treatment.
- Doxepin: Topical application of 5% Doxepin cream provides significant anti-itch effects in patients. Doxepin cream relieves itching and the side effects of the drug are temporary and mild, including burning at the site of application and drowsiness.
Other Forms of Therapy
- Topical antibiotic treatment as monotherapy or in combination with corticosteroids is effective if there is secondary infection.
- Cryotherapy with liquid nitrogen or CO2 is justified in the case of lesion infiltration. It has an anti-itch effect.
- Applications of trichloroacetic acid (10-33%) or podophyllin (2-10%) several times, depending on the duration of the lesion, reduce infiltration and relieve itching.
- In some cases, topical application of 0.05% tretinoin may have an effect.
Alternative and Experimental Treatment Methods
- Local PUVA therapy is recommended three times a week (3-5 J/cm2) for a total of 20 sessions.
- Bulgarian dermatologists have pioneered successful treatment of LSC with high-altitude climatotherapy. It reduces itching at altitudes of 2000 meters above sea level. The pathologically altered reactivity of the body is regulated to the level of hyposensitization. The beneficial effect of high-altitude climatotherapy is based on clean air, excess ultraviolet radiation, and low O2 pressure, which stimulate adrenal hormonal activity. (Low-evidence based)
- Acupuncture also helps relieve itching and may be recommended as supportive therapy. (Low-evidence based)
- Another common method to alleviate itching is cool or moderately cool baths.