Pemphigus is a group of bullous dermatoses in which the pathogenetic role is attributed to circulating autoantibodies against desmosomal antigens. ICD-10 code L10.
Development of pemphigus is observed in genetically predisposed individuals. The most significant association is with specific alleles of the major histocompatibility complex (HLA) genes. In different countries, there is a correlation with different alleles of genes encoding HLA. The disease may develop due to various factors (use of drugs containing thiol groups, exposure to sunlight, infectious agents, stress, consumption of certain foods, physical factors, etc.), but often it is not possible to determine the triggering factor.
Autoimmune processes result in the disruption of cell-cell adhesion in the epidermis (acantholysis) due to the formation of IgG autoantibodies against so-called "pemphigus" antigens (the most important of which are desmogleins 1 and 3) and their binding to glycoproteins. These immune complexes subsequently lead to the destruction of desmosomes and the formation of intraepidermal blisters.
The incidence of pemphigus in European and North American countries averages from 0.1 to 0.2 cases per 100,000 population per year.
Classification:
- L10.0 Pemphigus vulgaris
- L10.1 Pemphigus vegetans
- L10.2 Pemphigus foliaceus
- L10.3 Brazilian pemphigus
- L10.4 Pemphigus erythematosus (Senear-Usher syndrome)
- L10.5 Drug-induced pemphigus
- L10.8 Other types of pemphigus
- Paraneoplastic pemphigus
- IgA pemphigus
- Subcorneal pustular dermatosis
- Intraepidermal neutrophilic dermatosis
All clinical forms of pemphigus are characterized by a prolonged, chronic and fluctuating course, which, if left untreated, can lead to a deterioration in the patient's overall condition and, in some cases, even to a fatal outcome.
Pemphigus Vulgaris
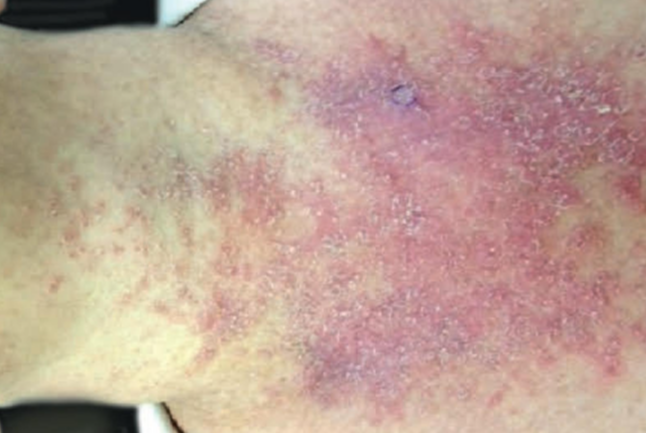
Pemphigus vulgaris is the most common form of the disease and is characterized by the presence of blisters of various sizes with thin, flaccid roofs containing serous fluid. These blisters may appear on apparently unaffected skin and/or mucous membranes of the oral cavity, nose, throat, and genitalia. Initial eruptions often occur on the mucous membranes of the mouth, nose, throat, and/or the red border of the lips. Patients experience pain when eating, speaking, and swallowing saliva. Hyper-salivation and a specific odor from the mouth are common symptoms. Within 3-12 months, the disease typically becomes more widespread and involves the skin.
The blisters last for a short time (from a few hours to a day). On mucous membranes, their appearance can sometimes go unnoticed because the thin roofs of the blisters rupture quickly, forming long-lasting, painful erosions. Some skin blisters may dry out and form crusts. Erosions in pemphigus vulgaris are usually bright pink with a shiny, moist surface. They tend to spread peripherally, and there may be generalized skin involvement with the formation of extensive areas of damage, deterioration of the patient's general condition, secondary infection, development of intoxication, and fatal outcome in the absence of therapy.
One of the most characteristic signs of pemphigus vulgaris is Nikolsky sign, which is a clinical manifestation of acantholysis and involves detachment of the epidermis upon mechanical manipulation of the skin in the affected areas and possibly in distant areas of the skin.
Pemphigus erythematosus (Senear-Usher Syndrome)
Unlike pemphigus vulgaris, which often begins with mucous membrane involvement, pemphigus erythematosus begins on seborrheic areas of the skin (face, back, chest, scalp). At the onset of the disease, erythematous areas with clear borders appear on the skin, with crusts of varying thickness, yellowish or brownish-brown in color, on their surface. The blisters are usually small and dry quickly to form crusts, exposing a moist, eroded surface when the crusts come away.
The blisters have a very thin, flaccid roof that is short-lived and often goes unnoticed by patients and physicians. Nikolsky sign is usually positive in areas of involvement. The disease may remain localized for many months or years, but it may spread to new areas of the skin and mucous membranes, most commonly in the oral cavity, causing symptoms similar to those of pemphigus vulgaris when the pathologic process becomes generalized.Pemphigus Foliaceus
Pemphigus vegetans
Pemphigus Vegetans is divided into two forms:
- Classical Form - Neumann Type
- Benign Form - Allopo Type
Clinical picture of Neumann-type pemphigus vegetans is characterized by involvement of the oral mucosa, skin folds and anogenital area. Vegetations may form on the surface of the erosions, which, when merging, may rise up to 1 cm above the level of the skin. Eruptions are usually accompanied by itching, pain and burning. After epithelialization of erosions, hyperpigmented spots remain.
Mucous membranes are less frequently involved in the Allopo-type of pemphigus vegetans. Eruptions are usually limited to intertriginous areas of the skin. Pustular and follicular elements may appear, forming plaques with vegetations. The course of this type is more favorable, with the possibility of remissions and, in rare cases, spontaneous recovery.
Pemphigus Herpetiformis
Pemphigus herpetiformis is a rare atypical bullous dermatosis that in some cases clinically resembles dermatitis herpetiformis. Eruptions may present as plaques with papules and vesicles at the periphery or as clusters of papules, vesicles or bullae similar to dermatitis herpetiformis.
Severe pruritus is characteristic of pemphigus herpetiformis. Without adequate treatment, the disease may progress and acquire features of pemphigus vulgaris or pemphigus foliaceus.Paraneoplastic Pemphigus
Paraneoplastic pemphigus occurs in the presence of neoplasia and may also develop during or shortly after chemotherapy for malignant tumors. In most cases, paraneoplastic pemphigus is associated with lymphoproliferative neoplasms, thymoma, sarcoma, carcinoma, and solid tumors at various sites.
Typically, the clinical presentation of paraneoplastic pemphigus is similar to that of pemphigus vulgaris, with concomitant skin and mucosal involvement. However, atypical pruritic skin lesions resembling erythema multiformis, bullous pemphigoid, or toxic epidermal necrolysis may sometimes be observed.Drug-induced pemphigus
IgA Pemphigus
IgA pemphigus is a rare group of autoimmune intraepidermal bullous dermatoses characterized by vesiculo-pustular eruptions, neutrophilic infiltration, acantholysis, and the presence of both fixed and circulating IgA autoantibodies directed against antigens of the intercellular adhesion substance of stratified squamous epithelium. The clinical presentation of IgA pemphigus, regardless of its manifestation, includes flaccid vesicles or pustules located on both hyperemic and apparently "healthy" skin.
Pustules tend to coalesce to form circular foci with crusts in the central part. Eruptions are most often localized in the axillary fossae, scrotum, trunk, upper and lower limbs. Less frequently, the pathological process involves the skin of the scalp and behind the ears, as well as mucous membranes. Patients often complain of severe pruritus. Typically, IgA pemphigus has a more benign course than IgG pemphigus.To establish a diagnosis, the following examinations are necessary:
- Clinical examination of the patient.
- Determination of Nikolsky sign.
- Tzanck smear test taken from the base of fresh erosions on mucous membranes and/or skin (the presence of acantholytic cells is not pathognomonic but is a crucial diagnostic sign; they may be absent at the beginning of the disease, especially in pemphigus erythematosus).
- Histological examination (to detect intraepidermal cleavage and/or blisters).
- Indirect immunofluorescence method (to detect circulating IgG autoantibodies against intercellular adhesion molecules). The patient's blood serum is used for this test.
- Direct immunofluorescence method (to detect IgG in a biopsy taken from seemingly healthy skin near the lesion site).
- Determination of antinuclear antibodies
Treatment Goals
- Stabilization of the pathological process.
- Prevention of new eruptions.
- Epithelialization of erosions.
- Achieving and maintaining remission.
- Improvement of the patients' quality of life.
General Remarks on Therapy
- The cornerstone of treatment for blistering disorders is systemic glucocorticosteroids, which are prescribed to any patient with a confirmed diagnosis. They are prescribed on the basis of clinical indications and there are no absolute contraindications to their use.
- In addition to glucocorticosteroids, adjuvant therapy (e.g., azathioprine, etc.) may be prescribed to reduce the dose or overcome resistance to glucocorticosteroids. Symptomatic therapy is used when indicated.
Systemic Therapy
Glucocorticosteroids
Prednisone is most commonly used, and other glucocorticosteroids (GCS) are prescribed according to their prednisone equivalent.
In the initial stage, treatment is with maximum doses of systemic GCS (80-100 mg per day, but not less than 1 mg per kg of the patient's body weight) for 3 weeks, occasionally 4 weeks or more. In severe cases, higher doses of GCS up to 200 mg per day or more may be prescribed. The medication is taken strictly in the morning (before 11:00). High GCS doses may be divided into two doses at 7:00-8:00 and 10:00-11:00, but always after meals. Oral administration of high GCS doses can be partially replaced by parenteral administration or extended-release forms of the drug (not more than once every 7-10 days). The criteria for assessing the positive effect of systemic glucocorticosteroid treatment in autoimmune blistering diseases include: absence of fresh bullous eruptions, epithelialization of 2/3 of lesions with ongoing active epithelialization of persistent erosive defects, especially those on the oral mucosa, a negative Nikolsky sign, and the absence of acantholytic cells.
The second phase of therapy is divided into 7 steps to gradually reduce the dose from 65 mg to 20 mg per day, corresponding to the average doses of systemic glucocorticosteroids for blistering disorders. This phase lasts for 9 weeks. The initial reduction of the GCS dose by 1/4 to 1/3 of the maximum dose is possible after achieving a clear therapeutic effect (cessation of new blisters, active epithelialization of erosions). It is not recommended to reduce the dose during active sun exposure, acute infectious diseases and exacerbations of chronic diseases.
In the third stage, the dose of systemic GCS is further reduced, starting at 20 mg per day.
Cytostatics
Used to enhance the effectiveness of GCS therapy and reduce its course dosage. Methotrexate at 20 mg (up to 25-30 mg if well tolerated) once weekly intramuscularly. The duration of therapy is individualized. During treatment, clinical and biochemical blood tests and urinalysis should be monitored at least 1-2 times per week.
Immunosuppressants: Used when GCS therapy is insufficiently effective and there are contraindications to the use of cytostatics.
Cyclosporine is administered orally at 5 mg per kg of body weight per day in two doses until a clinical effect is achieved, then the dose is reduced to the minimum maintenance dose. Cyclosporine treatment should be closely monitored for blood creatinine and urine creatinine.
Azathioprine
Azathioprine is prescribed at a daily dose of 100-200 mg orally. It is better tolerated by patients and rarely leads to complications. Azathioprine treatment should be closely monitored with complete blood count. Adjuvant azathioprine therapy for steroid resistance is administered in courses:
The first course is started while maintaining the maximum dose of systemic glucocorticosteroids - 150 mg of azathioprine per day for at least 1.5 months.
The second course begins with 10-8 tablets (50-40 mg) of systemic glucocorticosteroids per day, and the daily dose of azathioprine reaches 100 mg.
The third course begins with 4 tablets (20 mg) of systemic glucocorticosteroids per day, and the daily dose of azathioprine is 50 mg.
The fourth course involves administering azathioprine twice weekly at 50 mg each time after reaching the maintenance dose of systemic glucocorticosteroids.
Topical treatment
The area of blisters and erosions is treated with solutions of aniline dyes, and in the presence of secondary infection, aerosols containing glucocorticosteroids and antibacterial agents are used. Antiseptic solutions are used for rinsing erosions in the oral mucosa.
Nutrition
Frequent and small meals are recommended. If the oral cavity is affected, the patient's diet should include pureed soups to prevent complete food rejection. The diet should limit salt and carbohydrates while including protein and vitamins.
Outpatient management and preventive measures for autoimmune blistering disorders
When the patient's overall condition improves and there are no new bullous eruptions, or when there is complete or almost complete (2/3) epithelialization of erosive defects, patients with blistering disorders are transferred to outpatient management. After discharge from the hospital, these patients must remain under the supervision of a dermatologist and other relevant specialists.
The dose of systemic glucocorticosteroids is gradually reduced to a maintenance dose according to the schemes presented above, strictly under the control of a dermatologist. During the summer and viral epidemic periods, it is not advisable to reduce the dose of systemic glucocorticosteroids. Before undergoing surgery or dental prosthesis, the dose of systemic glucocorticosteroids should be increased by 1/3 of the daily dose for 3-5 days or a course of betamethasone injections (2 ml intramuscularly) should be administered 5 days before and after the planned surgery. Corrective therapy is mandatory.
Clinical examination and monitoring of laboratory parameters (urinalysis, complete blood count, blood biochemistry, coagulogram) should be performed at least twice a year, or more frequently if necessary. Annual monitoring includes blood electrolytes, chest x-ray, densitometry, abdominal ultrasound, renal ultrasound, thyroid ultrasound, pelvic ultrasound, mammography (for women), prostate examination (for men), esophagogastroduodenoscopy, tumor marker testing, and consultations with related specialists (internist, neurologist, endocrinologist, otolaryngologist, dentist, etc.).
Patients may be allowed to work in jobs that do not require excessive physical or mental stress and do not involve excessive exposure to cold or sunlight. Sunbathing is contraindicated in all forms of blistering disorders and it is important that patients consistently use sunscreens with maximum protection. Patients should follow a schedule of work, rest, and sleep. Change of climatic conditions and treatments with mineral waters and mud in spas, as well as therapeutic and cosmetic massages are not allowed.