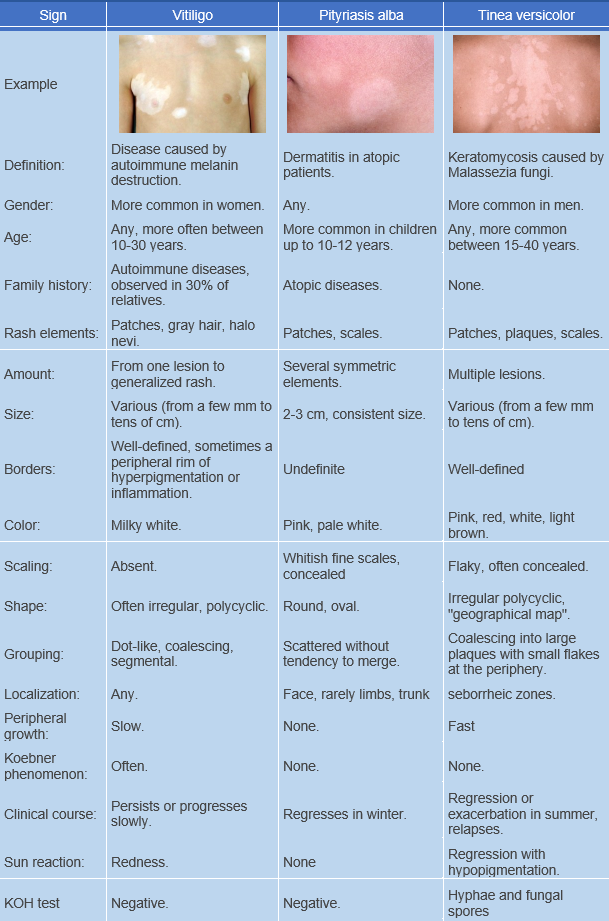
Tinea versicolor, also known as pityriasis versicolor, is a superficial fungal skin infection. ICD-10 code is B36.0.
This condition is prevalent worldwide, but is most common in regions with hot and humid climates. Prevalence ranges from 2% in moderate climates to 40% in tropical and subtropical regions. It primarily affects young and middle-aged individuals and rarely occurs in children and the elderly.
The causative agents of pityriasis versicolor are dimorphic lipophilic yeasts of the genus Malassezia, which are typical inhabitants of the skin microflora. The most common species are Malassezia globosa, M. sympodialis and M. furfur, and the less common species are M. slooffiae, M. restricta and M. obtusa. It has been established that approximately 90% of healthy individuals carry the saprophytic form of the fungus. Under the influence of predisposing factors of endogenous and/or exogenous nature, the pathogen transforms from the non-pathogenic budding yeast form to the pathogenic mycelial form.
Tinea versicolor is not contagious. Predisposing factors may include increased sweating and changes in the chemical composition of sweat. Pityriasis versicolor develops more often in individuals with concomitant conditions such as endocrine disorders, chronic lung and gastrointestinal diseases, autonomic-vascular disorders, various types of immunodeficiency, and others. Factors contributing to the development of the disease include nutritional deficiencies, oral contraceptive use, systemic glucocorticoids, and immunosuppressive drugs. There may also be a genetic (multifactorial) predisposition to the disease.
Classic Form
Skin eruptions are most common on the trunk and upper limbs, but can also affect the scalp and genital area. Atypical sites of pityriasis versicolor may include the face, earlobes, hands, shins, nipples, and periareolar region. In children, the condition often begins on the scalp, although the hair itself is not affected. Pityriasis versicolor does not occur on the palms, soles, or mucous membranes. The causative agent has a tropism for areas of the skin with a high concentration of sebaceous glands.
Initially, the disease presents with small, non-inflammatory, poorly defined patches. They begin as pink, then yellowish-pink, and later become brown or reddish-brown, with flaky, bran-like scales on their surface, which are easily seen when scraped. These patches are often multiple and may coalesce to form large lesions with polygonal borders; the size of the patches may vary from a few millimeters to several centimeters. Slight atrophy may sometimes be seen in the center of large lesions. As the lesions involute centrally, they may take on a ring-like appearance.
There is usually no subjective sensation, but occasionally mild pruritus may occur.Inverse Form
Hypopigmented Pityriasis Versicolor
Atrophic form
Diagnosis is usually based on the typical clinical presentation: characteristic eruptions on areas of skin covering the trunk and upper limbs.
Microscopic examination of scales treated with a 10-20% potassium hydroxide (KOH) solution for 20 minutes reveals fungal elements (short, curved hyphal threads - hyphae) in the form of "meatball-like" structures measuring 2 to 4 μm in diameter (large arrow) and large round and oval spores with a double-contoured shell clustered like grape clusters (small arrow).
Iodine test
Wood's lamp
The treatment of pityriasis versicolor is based on the use of antifungal agents both topical and systemic.
Topical treatment:
- Bifonazole, 1% cream or 1% solution once daily until clinical manifestations resolve (for 2-3 weeks) or
- Ketoconazole, cream once daily until clinical manifestations resolve (for 2-3 weeks) or
- Clotrimazole, cream or solution 1-2 times daily until clinical manifestations resolve (for 1-3 weeks) or
- Miconazole, cream twice daily until clinical manifestations resolve (for 3 weeks) or
- Terbinafine, cream and solution 1-2 times daily until clinical manifestations resolve (for 3 weeks) or
- Oxiconazole, cream 1-2 times daily until clinical manifestations resolve (for 2 weeks).
Systemic treatment:
Systemic antifungals are prescribed for widespread and atypical forms of pityriasis versicolor or when topical therapy is ineffective for localized lesions:
- Ketoconazole 200 mg orally once daily daily for 3-5 weeks or
- Itraconazole 200 mg orally once daily for 1 week or 100 mg orally once daily after a meal for 15 days (if isolated eruptions persist after a 2-week break, a repeat treatment course at the same dose is recommended) or
- Fluconazole 300 mg orally once a week for 2 weeks or 150 mg orally once a week for 4 weeks.
Prevention:
As a preventive measure for individuals predisposed to recurrent pityriasis versicolor, it is advisable to take ketoconazole at a dose of 400 mg per month or 200 mg for three consecutive days per month, or itraconazole at a dose of 400 mg once a month for 6 months.