Rosacea is a chronic inflammatory skin disease that causes redness and a rash, usually on the nose and cheeks. ICD-10 code: L71.
The condition more commonly develops in women 30-50 years old who have a specific genetic predisposition to transient flushing on the face, less commonly on the neck and cleavage area. It is occasionally observed in children, adolescents and the elderly. It is believed that individuals with phototypes 1 and 2 are more susceptible to this dermatosis, but it can occur in individuals with any skin phototype. In men, severe complications such as rhinophyma are more common, whereas in women, despite a relatively milder course, rosacea often leads to serious psychological and emotional disturbance.
The prevalence of rosacea ranges from 1.5% to 10% in European countries, and there are 14 million registered cases in the United States.
Rosacea is considered an angioneurosis, primarily localized in the area innervated by the trigeminal nerve, and is caused by various factors that can be grouped into the following categories:
- Vascular disturbances; Changes in dermal connective tissue
- Microorganisms
- Immune disorders
- Changes in the sebaceous and hair follicle
- Oxidative stress
- Climatic factors
- Psychovegetative disorders
Factors contributing to the development of rosacea include:
- Constitutional angiopathy
- Emotional stress
- Hormonal imbalances
- Exposure to chemical agents
Recently, the role of cathelicidins in the pathogenesis of rosacea has received much attention. Cathelicidins are a family of multifunctional proteins that protect the skin from infectious agents, modulate local inflammatory responses and angiogenesis through direct effects on endothelial cells and immunity. In patients with rosacea, the levels of cathelicidins in the facial skin and proteases in the stratum corneum are significantly increased.
The association with Bacillus oleronius, a bacterium isolated from Demodex mites that interacts with peptides to stimulate inflammatory responses in individuals with papulopustular rosacea, is being investigated. Epidermal Staphylococcus is thought to play an etiological role in the pathogenesis of pustular and ocular rosacea, possibly related to the expression of its pathogenic properties due to facial vasodilation. The relationship between rosacea and Helicobacter pylori has also been discussed.
Pre-rosacea
Erythemato-telangiectatic rosacea
This subtype is characterized by development of persistent erythema primarily on the cheeks and sides of the nose. The color of erythema may vary from bright pink to bluish red, depending on the duration of the disease. Telangiectasias of various diameters and skin swelling also occur in patients with this condition.
Most patients complain of burning and tingling sensations in the area of erythema. The condition worsens with exposure to low and high temperatures, alcohol, spicy foods, and emotional stress. Increased skin sensitivity to topical medications and ultraviolet radiation is characteristic. Even indifferent creams and sunscreens may aggravate inflammation.Papulopustular rosacea
This subtype is characterized by bright red papulopustular eruptions with perifollicular distribution that develop against a background of persistent erythema and telangiectasias. Periorbital erythema and scaling are usually absent. Facial skin becomes swollen and porous. Comedones are absent. Skin sensitivity to sunlight is markedly increased.
Subjective sensations (such as burning or tingling) are usually not pronounced. Gradually, the persistent papulopustular eruptions cover the entire facial surface, appear on the scalp, neck, retroauricular folds, central part of the chest, and less frequently on the back. Eruptions on the head are accompanied by pruritus.Rosacea Conglobata
Rosacea Fulminans
Gram-negative rosacea
Develops after long-term systemic and topical antibiotic therapy for rosacea, primarily from tetracycline class. Eruptions often occur 2-4 weeks after completion of antibiotic therapy. The destruction of the gram-positive flora leads to the colonization by gram-negative bacteria.
In the follicular form of the disease, pustules 2-3 mm in diameter appear on the cheeks, nasolabial folds, and chin against a background of erythema and infiltration. Bacteriologic examination of pustular contents reveals Escherichia coli and Enterobacter, Klebsiella and Pseudomonas.
The cystic form is characterized by bluish-red papules, small nodules and cysts caused by Proteus mirabilis. Gram-negative rosacea is highly resistant to further treatment.Morbihan Disease
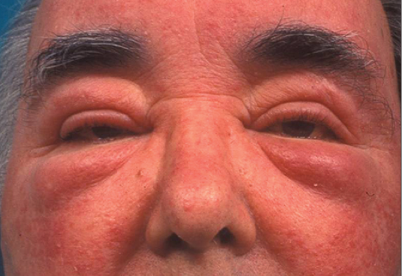
Also known as rosacea with solid persistent edema and rosacealymphedema, this condition is more common in men and is extremely rare. The etiology is still unknown, but it is believed to be allergic in origin.
It begins with bright pink erythema, isolated papules, and telangiectasias. Gradually, the intensity of the erythema increases and a persistent, dense swelling of the upper half of the face (forehead, eyelids, nose) develops, caused by lymphostasis and fibrosis, which gradually worsens without subjective sensations. Palpation of the affected areas reveals density, and there are no depressions on pressure.Phymatous rosacea
Characterized by significant thickening of the tissue and uneven roughness of the skin surface. The appearance of such changes on the skin of the nose is called rhinophyma, on the forehead - metophyma, on the chin - gnathophyma, on the earlobes (which can be unilateral) - otophyma. Much less frequently, the process spreads to the skin of the eyelids (blepharophyma). Rhinophyma occurs almost exclusively in males. Four histopathologic variants of nodular formations are distinguished: glandular (sebaceous), fibrous, fibrous-angiomatous, actinic.
In the glandular form, the nose shows bumpy or lobulated, soft, bluish-red growths with multiple dilated openings of sebaceous glands and telangiectasias.
Fibrous rhinophyma is characterized by bluish-purple skin color of the nose, multiple telangiectasias, and density of the affected areas on palpation. There is marked hyperplasia of the sebaceous glands, giving the skin a fine-grained appearance, which gradually leads to disfiguring deformity of the nose.
Fibro-angiomatous rhinophyma is clinically similar to fibrous rhinophyma and differs only in the lower density of elements. The surface of the nose has a dark red color due to numerous telangiectasias. In contrast to the fibrous stage, there are numerous superficial and deep pustules. The contents of the pustules dry to form purulent crusts. Patients complain of paresthesia, pruritus, and tenderness.
Actinic rhinophyma is characterized by a uniform and moderate enlargement of the nose, which gradually acquires a brownish-blue color with telangiectasias localized on the nostrils. The openings of the sebaceous glands are dilated and pustules are absent.Ocular rosacea
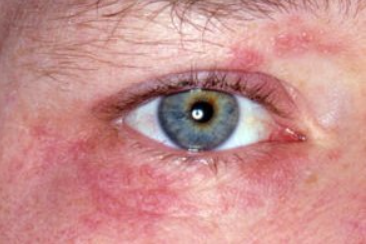
The frequency of eye involvement in rosacea ranges from 20% to 60%. It is more common in women than in men. It may be associated with facial skin lesions or, less commonly, occur as an isolated phenomenon. It is more common in individuals with the papulopustular type of rosacea and less common in the erythematotelangiectatic and phymatous types. It manifests as blepharitis, conjunctivitis, iritis, iridocyclitis, keratitis and the formation of often multiple chalazia.
Blepharitis is the most common symptom of rosacea. The eyelids become swollen, hyperemic and sometimes covered with small whitish scales. Patients complain of itching, the appearance of discharge in the corners of the eyes, especially in the morning, and a "gritty" sensation in the eyes that leads to frequent blinking.
Conjunctivitis in rosacea often coexists with blepharitis and is characterized by conjunctival hyperemia, pronounced tearing in wind and sunlight.<.p>
Iritis is rare. Patients complain of pronounced tearing and decreased visual acuity. The pattern of the iris becomes blurred, its color changes, and the pupil narrows.
Iridocyclitis involves inflammation of the ciliary body, as evidenced by the onset of pain.
Keratitis in rosacea begins with dilation of the peripheral scleral vessels, which gradually evolve into perivascular infiltrates, as in skin lesions. Inflammatory infiltrates slowly advance into the central regions of the cornea and undergo disintegration. Clinically, this is characterized by ulceration followed by scarring. Calcium salts deposited in connective tissue scars give the areas of opacification a whitish appearance. Progressive loss of visual acuity may lead to blindness.
Inflammation of the meibomian gland (chalazion) forms slowly, often painlessly. Initially, there is hyperemia, and under the skin, a mobile formation the size of a poppy seed to a pea can be palpated adhering to the cartilage of the eyelid.Granulomatous Rosacea
Steroid Rosacea
Rosacea Induced by Calcineurin Inhibitors
Rosacea Induced by Amiodarone
Halogenic Rosacea
Rosacea Induced by Vitamin B
Rosacea Induced by Calcium Channel Blockers
Rosacea Induced by Selective Phosphodiesterase Inhibitors
Rosacea Induced by Epidermal Growth Factor Receptor Inhibitors
Rosacea-like id reaction
Haber's Syndrome
Diagnostic criteria for rosacea (National Rosacea Society, 2002)
Primary:
- Persistent erythema.
- Transient erythema.
- Papules/pustules.
- Telangiectasia.
Secondary:
- Burning/stinging/swelling sensations
- Dry skin and scaling
- "Ocular" symptoms.
- Phymatous changes.
- Erythematoud plaques
- Peripheral location
At least two criteria are required for diagnosis.
Diagnostic criteria for rosacea in children
Rosacea in children is rare and occurs in individuals with skin phototypes 1-2. In children, facial flushing lasting more than 30 minutes after school activities is considered a risk factor for developing rosacea at an older age.
- Transient or persistent erythema.
- Telangiectasia.
- Papules and pustules without comedones.
- Predominantly located on the face.
- Eye involvement (one of the following signs: recurrent chalazion, hyperemia, keratitis).
At least two criteria are required for diagnosis.
Demodex mite examination
The specimen should be examined within the first few minutes after collection, as mites become more mobile and disintegrate over time. Transparent, elongated, mobile mites and larvae are found under the microscope. Their movements, especially the movement of the four short legs on each side of the body, help to identify the parasite.
Pre-rosacea and erythemato-telangiectatic rosacea:
- Carcinoid syndrome (pheochromocytoma, medullary thyroid cancer)
- Blushing syndrome
- Erythema from alcohol consumption
- Erysipelas
- Pellagra
- Menopause
- Chronic actinic dermatitis
- Frey's syndrome
- Polycythemia vera
- Discoid lupus erythematosus
- Seborrheic dermatitis
- Dermatomyositis
- Photoallergic and phototoxic reactions
- Cellulitis
- Mastocytosis
Papulopustular Rosacea
- Acne vulgaris
- Perioral Dermatitis
- Acne Conglobata
- Gram-Negative Folliculitis
- Pityrosporum Folliculitis
- Pseudomonas Folliculitis
- Eosinophilic Folliculitis
- Bacterial Folliculitis
Phymatous Rosacea
- Sarcoidosis
- Basal Cell Carcinoma
- Squamous Cell Carcinoma
- Granulosis rubra nasi
- Sebaceous Carcinoma
- Angiosarcoma
- Leprosy
- Melkersson-Rosenthal Syndrome
Ocular Rosacea
- Chronic Blepharitis
- Hordeolum and Chalazion
- Chlamydial Conjunctivitis
- Dry Eye Syndrome
- Keratitis
- Cicatricial Pemphigoid
Granulomatous Rosacea
- Lupus miliaris disseminatus faciei
- Sarcoidosis
- Granulomatous Perioral Dermatitis
General Treatment Notes
- The therapeutic approach depends largely on the clinical subtype of the disease. However, the success of rosacea treatment is based on the combined efforts of the physician and the patient to identify the triggering factors, which are strictly individual. These factors often include meteorological factors: exposure to sunlight, high and low temperatures, wind and associated abrasive effects; dietary factors: consumption of hot and carbonated drinks, alcohol, spicy foods and excessive food intake; neuroendocrine factors: Neuroendocrine factors: emotional stress, menopausal syndrome, and endocrinopathies associated with increased blood flow; Iatrogenic factors: both systemic medications that cause facial erythema and topical preparations, including cosmetic products and cleansers with irritating effects (waterproof cosmetics and toners that require the use of solvents, as well as cleansers containing soap). Eliminating or reducing the effects of these factors significantly influences disease progression and reduces the need for medication.
- The basis of therapeutic measures is adequate daily skin care. This includes, first and foremost, the use of sunscreens, which should be chosen with the increased sensitivity of the skin in rosacea patients in mind. Indifferent preparations (titanium dioxide, zinc oxide), which block ultraviolet radiation of the skin due to their physical properties, have the least irritating effect. Products with chemical UV filters, which can be recommended to rosacea patients, should not contain sodium lauryl sulfate, menthol and camphor, but should contain silicones (dimethicone, cyclomethicone), which significantly reduce the irritating effect of sunscreens, provide water resistance and low comedogenicity.
- Daily skin care recommendations should include the use of light textured concealers for daily use. It is advisable to apply them in a thin layer 1-2 times per day and as a base for makeup, preferably in the form of a powder or a shaken mixture. It has been shown that the use of concealers does not worsen the course of rosacea and can have a positive impact on the quality of life of patients. Restoring the skin's barrier function is an important component of rosacea therapy.
- Topical treatment is preferred for all types of rosacea except phymatous rosacea, for which surgery and systemic retinoids are most effective.
- In erythemato-telangiectatic subtype, azelaic acid and lasers are used.
- In papulopustular rosacea, mild to moderate severity, recommended treatments include azelaic acid, ivermectin, metronidazole, or a short course of antibiotics.
- In severe cases of papulopustular rosacea, a 4-week course of doxycycline followed by a 50% dose reduction is recommended. Low-dose isotretinoin is also indicated.
- For initial manifestations of the phymatous subtype of rosacea, isotretinoin monotherapy is most effective, and surgical excision of affected tissue may be required later.
- Treatment recommendations for ocular rosacea include topical fusidic acid and metronidazole at the eyelid margins, systemic tetracyclines, and artificial tears.
Systemic Treatment
Antibacterial Drugs:
- Doxycycline (drug of choice): 100-200 mg per day orally for 14-21 days, maintenance dose of 100 mg per day for 12 weeks.
- Erythromycin (alternative drug): 0.25 mg four times a day orally for 14-21 days (possible up to 28 days).
- Clarithromycin (alternative drug): 500 mg per day orally for 14-21 days (possible up to 28 days).
5-Nitroimidazole Group Drugs (alternative drugs in case of intolerance or ineffectiveness of antibacterial therapy):
- Metronidazole: 1.0-1.5 g per day orally for 4-6 weeks (possible up to 8 weeks).
Systemic Retinoids (for severe, treatment-resistant rosacea):
- Isotretinoin 0.1-0.3 mg per kg of body weight orally once a day after a meal for 4-6 months
Monthly monitoring of biochemical parameters (total bilirubin, ALT, AST, triglycerides, total cholesterol, glucose, creatinine, alkaline phosphatase) is mandatory before prescribing and during treatment. The drug is a potential teratogen and has side effects. The safety data for isotretinoin have allowed the following key points to be formulated: a standard 20-week course of isotretinoin treatment is usually well tolerated and safe; skin and mucosal side effects are common, reversible, respond well to local moisturizing therapy, and do not require discontinuation of the drug; musculoskeletal side effects are rare; minor laboratory abnormalities are occasionally observed that do not require discontinuation of the drug. Liver function and lipid metabolism parameters should be analyzed after 2-4 weeks; the contraceptive period after treatment is 1 month. Isotretinoin intake by men does not affect spermatogenesis.
Topical treatment
- Metronidazole, 0.75% gel or 1% cream, is applied in a thin layer to cleansed skin twice daily, morning and evening, for 3-9 weeks. An occlusive dressing may be used if necessary. Cream and gel may be used alternately. The average course of treatment is 3-4 months.
- Azelaic acid, 15% cream or gel, is applied to all affected areas of the skin and gently rubbed in twice daily (morning and evening). Approximately 2.5 cm of cream is sufficient for the entire face. Improvement is usually seen after 4 weeks of treatment. However, for best results, it is recommended to continue using the product for several months.
- Clindamycin phosphate 1% gel or clindamycin hydrochloride 1% solution for external use. A thin layer of gel or solution is applied twice daily to the affected skin area, which should be cleansed and dried. The course of treatment should not exceed 6-8 weeks.
- Topical Calcineurin Inhibitors:
- Tacrolimus is effective in reducing erythema but not papulopustular eruptions in papulopustular rosacea: 0.03% or 0.1% tacrolimus ointment and 1% pimecrolimus cream are effective in cases of steroid dependence.
- Tacrolimus, 0.03% ointment and 0.1% ointment, should be applied in a thin layer to the affected areas of skin. Treatment should begin with 0.1% ointment twice daily and continue until lesions are completely cleared. As the skin condition improves, reduce the frequency of application or switch to 0.03% ointment. Improvement is usually seen within one week of starting therapy. If there is no improvement in symptoms within two weeks of therapy, consider changing the therapeutic strategy.
- Pimecrolimus, 1% cream: Apply a thin layer of cream to the affected area twice daily and massage gently until completely absorbed. Emollients may be applied immediately after cream application. However, after showering, emollients should be applied before applying the cream.
- Encapsulated Benzoyl Peroxide Cream: Lightly massage a pea-sized amount of cream onto each area of your face (forehead, chin, nose, and cheeks). Avoid your eyes, lips, and mouth.
- Topical Retinoids: Apply adapalene, 0.1% cream or gel once daily at night to clean, dry skin over the entire affected area, avoiding contact with eyes and lips. Therapeutic effects develop after 4-8 weeks of treatment and sustained improvement after 3 months of treatment. If necessary, the course of treatment can be extended. In some cases, due to transient skin irritation, the number of applications may be reduced or treatment may be interrupted until signs of irritation disappear.
- Brimonidine: Mirvaso gel is indicated for the erythematous stage of rosacea, which is characterized by persistent facial flushing. The medication is applied once daily, usually in the morning, for several months.
- Ivermectin: Soolantra 1% Cream. Prescribed for the papulopustular stage of rosacea. Apply once daily to the skin in each of the five facial areas: forehead, chin, nose, and cheeks, and spread over the entire face, avoiding the eye and lip areas. Treatment may be continued for up to 4 months.
Non-Medication Therapy
Non-coherent intense pulsed light (IPL) and diode, KTP, alexandrite, and the most modern long-pulse neodymium-doped yttrium-aluminum-garnet (Nd:YAG) lasers are used in the treatment of rosacea. In the treatment of the hypertrophic type of rosacea, laser dermabrasion is one of the leading procedures due to its safety. Microcurrent therapy is also widely used as a physiotherapeutic treatment. Cryotherapy is used, which can have anti-inflammatory, vasoconstrictive and anti-demodex effects. The procedure is performed 2-3 times a week for a course of 10 sessions. This recommendation is supported by few clinical observations and opinions of individual experts. Overall, studies on the efficacy of physical methods for the treatment of rosacea are mostly descriptive.
Supportive treatment for rosacea
Considering that rosacea is a chronic inflammatory dermatosis, maintenance therapy after primary treatment is indicated: metronidazole 0.75% gel applied externally twice a week for 6 months or azelaic acid 15% gel applied twice a day for 6 months.
Treatment for pregnant women
Topical azelaic acid in combination with topical erythromycin is recommended. In severe forms of rosacea, systemic erythromycin may be considered.
Prevention
Prevention of rosacea flares involves limiting or avoiding triggering factors, including meteorological factors, sun exposure, certain foods, drinks and pharmacological agents that induce facial erythema, as well as aggressive cosmetic procedures (physical and chemical peels, dermabrasion, abrasive treatments, thermoactive masks, etc.). Patients are advised to use gentle skin care with mild cleansing, moisturizing and photoprotective products designed for sensitive skin. Supportive therapy with topical metronidazole or azelaic acid is recommended.