Pityriasis Rosea - an acute, self-resolving inflammatory dermatosis characterized by typical oval or coin-shaped maculopapular and erythematous-squamous lesions. ICD-10 Code: L42
The prevalence of the condition ranges from 0.4% to 4% of all skin conditions, and is more common in females than males by a ratio of 3:2. Pityriasis rosea is seen predominantly in adolescents and young adults, with rare occurrences in older adults and young children.
The cause of the disease is unknown. There is a widely accepted hypothesis suggesting an infectious, primarily viral, origin. In recent years, particular attention has been paid to the role of human herpesviruses 6 and 7 in the development of the disease; however, the etiologic agent has not been conclusively identified. Seasonal variations in incidence, the presence of prodromal symptoms in some patients, and the characteristic course of the disease are indirect evidence of its infectious nature.Classic Pityriasis Rosea
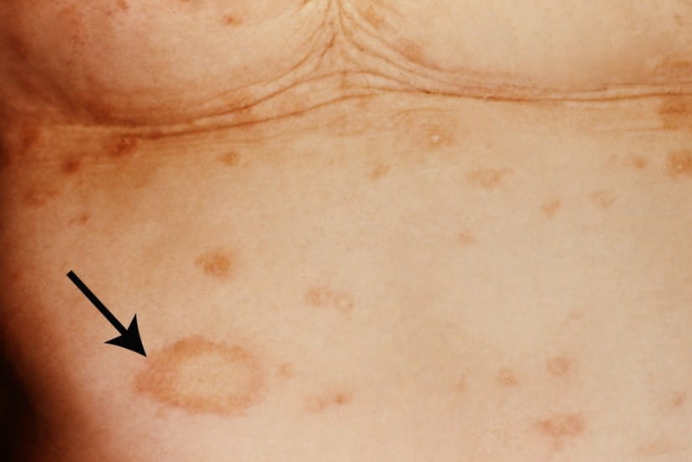
In 80% of cases, a bright, oval, slightly raised "herald" patch 2 to 5 cm in diameter appears at the onset of the disease, usually on the trunk. The center of the herald patch shows scaling. One to two weeks later, multiple edematous, pinkish erythematous-squamous patches appear, 2-3 cm in diameter, typically round or oval in shape, arranged along the lines of Langer (on the back, resembling a "Christmas tree" pattern). The central portion of these patches is delicately folded, sometimes pigmented, and associated with scaling. The scaling is more pronounced at the border between the central and peripheral zones.
In 20% of cases, the "herald" patch is absent, or multiple "herald" patches may be present. In rare cases, the "herald" patch is the only skin lesion ("unheaded" pityriasis rosea).
The lesions do not appear simultaneously, resulting in an evolving polymorphism. The lesions begin to dissolve from the central part, which is pigmented, loses its bright color and begins to desquamate. The ring of erythema gradually disappears, leaving a mild hyperpigmentation.
Pityriasis rosea does not usually recur. Spontaneous healing occurs around the 4th to 5th week of the disease. Residual clinical manifestations are uncommon. In some cases, hypo- or hyperpigmentation may occur, often exacerbated by sun exposure or ultraviolet therapy.Irritated Pityriasis Rosea
Pityriasis Circinata et Marginata of Vidal
Pityriasis Rosea-like Drug Eruptions
- ACE inhibitors
- Isotretinoin
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Omeprazole
- Terbinafine
- Tyrosine kinase inhibitors
Atypical Forms of Pityriasis Rosea
The diagnosis is based on the patient's history (association with a recent infection, exposure to cold, general health disturbance) and the clinical presentation of the disease (presence of the "Herald patch", erythematous-squamous elements arranged along Langer's lines).
Diagnostic criteria (Chuh A.A. 2003):
Main criteria:
- Isolated eruptions with a ring-shaped or round form.
- Scaly surface of the lesions.
- Peripheral scaling in the form of a "collarette."
Additional criteria:
- Localization on the trunk and proximal areas.
- Arrangement along Langer's lines of skin tension.
- Presence of "herald patch" preceding the eruptions.
Laboratory tests:
- Routine compete blood count and urinalysis tests.
- Serological tests to rule out syphilis.
- Microscopic examination of skin scrapings to rule out fungal infections.
- Nummular Eczema
- Psoriasis
- Pityriasis Lichenoides
- Small Plaque Parapsoriasis
- Large plaque parapsoriasis
- Syphilitic Roseola
- Papular Syphilis
- Tinea Corporis
Spontaneous healing usually occurs within 4-5 weeks of the onset of the disease. Uncomplicated cases of pityriasis rosea do not require treatment.
Treatment is indicated for generalized skin involvement, significant exudative eruptions, allergic reactions, or pruritus.
For widespread skin involvement accompanied by severe itching:
Topical glucocorticosteroids:
- Hydrocortisone butyrate cream or ointment 0.1%, applied 1-2 times daily for 5-7 days.
- Alclometasone dipropionate cream or ointment 0.05%, applied 1-2 times daily for 5-7 days.
- Methylprednisolone aceponate cream or ointment 0.1%, applied 1-2 times daily for 5-7 days.
- Mometasone furoate cream or ointment 0.1%, applied 1-2 times daily for 5-7 days.
Antihistamines:
- Cetirizine hydrochloride: Adults and children over 6 years old, a daily dose of 10 mg orally for adults (1 dose) and 5 mg orally twice a day for children for 7-10 days.
- Loratadine: Adults and children over 12 years old, 10 mg orally once a day; for children aged 3 to 12 years with a body weight less than 30 kg, 5 mg orally once a day, and for children with a body weight over 30 kg, 10 mg orally once a day for 7-10 days.
- Chloropyramine: For children aged 1 to 6 years, 8.3 mg orally 2-3 times a day; for children aged 6 to 14 years, 12.5 mg orally 2-3 times a day; for adults, 25 mg orally 3-4 times a day for 7-10 days.
- Clemastine: For children over 7 years old, 0.5-1 mg orally twice a day; for adults, 1 mg orally twice a day for 7-10 days.
In complicated forms of the disease, systemic glucocorticosteroid may be prescribed:
- Prednisone 15-20 mg daily orally until symptoms are alleviated.