Confluent and reticulated papillomatosis of Gougerot and Carteaud (CARP) is a rare disorder of epidermal keratinization characterized by the development of hyperkeratotic papules that coalesce into continuous and reticulated plaques. Its ICD-10 code is L85.9.
It primarily affects young women (with an average age of 19 years) with darker skin tones. The pathogenesis of CRP is not well understood, but a leading theory suggests an abnormal immune response to yeast-like fungi of the genus Malassezia and/or the gram-positive actinomycete Dierzia papillomatosis, leading to a disturbance in keratinocyte differentiation. Support for this theory comes from the fact that the disease has responded to antifungal (imidazoles) and antibacterial (tetracyclines and macrolides) medications. However, these microorganisms are not detected in all cases (approximately 50% of cases).
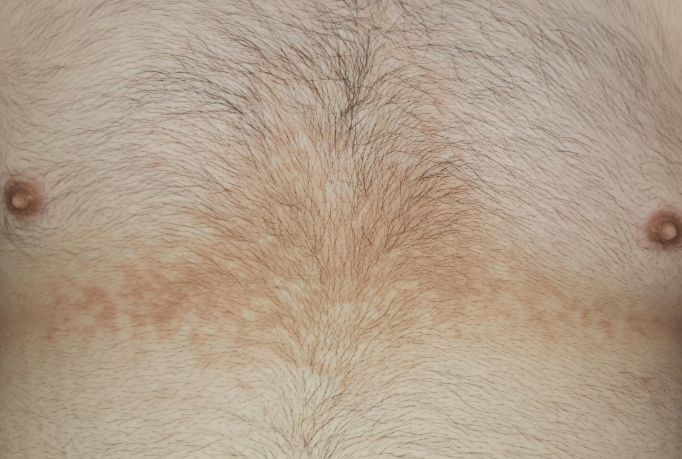
There have been reports linking papillomatosis to obesity, insulin resistance, thyroid dysfunction, and Cushing's disease. Rare familial cases have been described, suggesting possible genetic factors.The disease typically begins with the appearance of erythematous or pigmented, small (1-2 mm) hyperkeratotic papules on the trunk. Over a period of weeks to months, these papules enlarge and coalesce into plaques that may be pink, red, gray, or brown, with intricate polycyclic borders and a reticulated pattern at the periphery. The skin over the plaques is infiltrated and has an accentuated texture that is difficult to pinch.
The eruptions usually first appear on the chest and then spread centrifugally to the abdomen. In rarer cases, the face (often behind the ears), neck (posterior aspect), back (interscapular region), shoulders, armpits, groin folds, and extremities (often the elbow folds) may be affected.
Localized forms affecting only the face or pubic area have been reported. Mucous membranes are not involved and pruritus is usually absent or minimal.The diagnosis is based on a characteristic clinical presentation, medical history, and histologic examination showing hyperkeratosis, acanthosis, papillomatosis, thinning of the granular layer, proliferation of blood vessels in the papillary layer, and perivascular lymphocytic infiltration in the dermis. A potassium hydroxide (KOH) test and culture are recommended to rule out (confirm) fungal and bacterial infections.
Diagnostic criteria (Davis, 2006):
- Brown spots and plaques with scaling, some of which are arranged in a reticular pattern and have a papillomatous surface.
- Predominant localization of the rash on the neck and upper trunk.
- Negative KOH test for fungi.
- No response to antifungal therapy.
- Good therapeutic response to minocycline.
- Pityriasis versicolor.
- Flat warts.
- Hyperkeratosis due to poor personal hygiene.
- Acanthosis nigricans.
- Macular amyloidosis.
- Prurigo pigmetosa
- Darier disease.
- Seborrheic keratosis
- Erythrokeratodermia variabilis.
- Dermatopathia pigmentosa reticularis
- Epidermodysplasia verruciformis (Levandovsky-Lutz syndrome).
- Erythema dyschromicum perstans
- Erythema ab igne.
- Dowling-Degos disease.
- Congenital dyskeratosis.
First-line therapy:
- Minocycline 50-100 mg twice daily (p.o. - oral administration).
- Azithromycin 250-500 mg three times a week.
- Clarithromycin 500 mg once daily.
- Erythromycin 1,000 mg daily.
- Tetracycline 500 mg twice daily.
- Topical: Mupirocin ointment twice daily.
Second-line therapy:
- Selenium sulfide shampoo (or paste) for 10 minutes daily.
- Ketoconazole (cream or shampoo) twice daily.
- Calcipotriol 0.005% cream twice daily.
Third-line therapy:
- Tretinoin cream (0.025%, 0.05%, 0.1%) - at night.
- Tazarotene cream - at night.
- Isotretinoin 0.5-1 mg/kg divided into two daily doses.