Drug eruption is an acute inflammatory skin condition, and sometimes mucous membranes, that develops due to the hematogenous spread of an allergen. ICD-10 code: L27
Drug eruption more often develops as a side effect of medications. The pathological reaction can occur with any medication, including antihistamines and glucocorticoids. In most cases, however, drug eruption is associated with the use of antibiotics from the penicillin and cephalosporin groups, as well as sulfonamides, antiepileptic drugs, and allopurinol. The development of such eruptions is associated with the predominance of CD4 and CD8 T lymphocytes and delayed-type hypersensitivity.
Alimentary (food) eruptions can be caused by both allergic (common in children and rare in adults) and non-allergic mechanisms, accounting for 12% of all cases according to modern research.
Urticaria and angioedema are usually associated with IgE-mediated reactions and may be related to the use of medications, most commonly beta-lactam antibiotics.
Fixed drug eruptions are typically caused by delayed-type hypersensitivity. The development of eruptions occurs hours after exposure to the allergen. Common causes of such eruptions include tetracyclines, nonsteroidal anti-inflammatory drugs, sulfonamides, and antiepileptic drugs (e.g., carbamazepine).
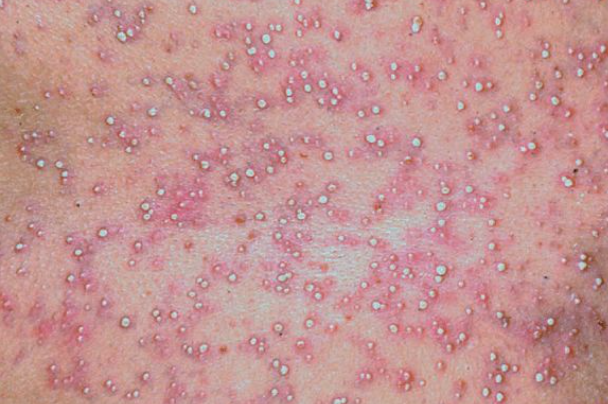
Pustular eruptions are currently rare because they are associated with the ingestion of rarely used halogen compounds.
Bullous eruptions, including drug-induced bullous dermatoses, are not common but represent severe forms of drug eruption. Their development is associated with the activation of enzymes and cytokines, leading to the formation of autoantibodies that promote acantholysis or epidermolysis. Angiotensin-converting enzyme inhibitors, furosemide, penicillin, and sulfasalazine are the most common causes of such reactions.
Drug-induced erythema multiforme is most commonly associated with the use of sulfonamides. The most common causes of maculopapular, erythematous, and hemorrhagic eruptions are antibiotics of the penicillin and cephalosporin groups. Hemorrhagic eruptions may also occur after taking antipyrine, salicylates, belladonna, quinine, ergotamine, and some other drugs.
Occupational drug eruptions occur due to exposure to industrial chemicals, especially those containing a benzene ring with chlorine or an amino group in their structure (which have high antigenic activity). The route of entry into the body is often inhalation.
The list of drugs that cause photochemical drug eruption exceeds 100 names and is constantly expanding. Among them, the most common are Antibiotics (amoxicillin, griseofulvin, dapsone, sulfonamides, oxytetracycline, tetracycline, doxycycline, minocycline, sulfonamides, ciprofloxacin), non-steroidal anti-inflammatory drugs (diclofenac, ibuprofen, indomethacin, ketoprofen, piroxicam, phenylbutazone), cancer drugs (vinblastine, methotrexate, fluorouracil), diuretics (amiloride, hydrochlorothiazide, furosemide, chlorthiazide), antihypertensive and cardiovascular agents (beta-adrenergic blockers, captopril, cordarone, methyldopa, nifedipine), oral antidiabetic agents (tolbutamide, chlorpropamide), and amitriptyline, benzoyl peroxide, isotretinoin, tretinoin, etretinate, promethazine, gold preparations, oral contraceptives, cimetidine, chlorpromazine, quinine, para-aminobenzoic acid esters, and others.
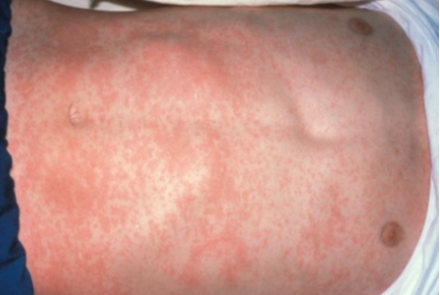
The onset of a reaction to a pharmacological agent occurs between 1 and 21 days and depends on the previous contact with this drug (or drugs with a similar chemical structure in the case of cross-reactivity). An early reaction occurs within 1-3 days of starting treatment, while a late reaction typically occurs around day 9-10 in non-sensitized patients. A reaction to penicillin can sometimes be observed two weeks or more after discontinuing its use.Maculopapular drug eruption
Maculopapular drug eruption, presenting as erythematous, pigmented, or hemorrhagic (purpuric) elements, is more common than other forms and typically occurs on the trunk, face, and limbs. The rash often coalesces in large skin folds (groin, axilla, under the breasts). The distribution of the eruptions may range from isolated lesions to erythroderma. The surface of the lesions is smooth, and later desquamation may occur. Sometimes the center of a growing patch becomes paler than the periphery, giving the elements a ring-like appearance. Pruritus of variable intensity is a common feature. Concomitant symptoms may include scleral injection, lacrimation, gastrointestinal upset, and a slight increase in body temperature. The eruptions may occur at different times after taking the drug, sometimes very rapidly if hypersensitivity to the drug has previously developed. They may appear immediately or gradually, in waves, reaching their maximum development within 2-3 days and disappearing after a few days without leaving any traces. If the palms and soles are affected, complete peeling of the horny layer occurs.
Macular erythematous and purpuric elements, similar to those seen in scarlet fever, occur less frequently. The process lasts a considerable time and ends with lamellar desquamation.Fixed drug eruption
Bullous drug eruption
Pustular drug eruption
Urticaria and angioedema
The following information is gathered: the presence of similar symptoms in the patient's medical history, the presence of occupational risk factors for the development of the condition, the use of medications, and so on. Many patients do not consider certain products they have been using for a long time (nasal or eye drops, birth control, supplements) to be medications. Patients also typically do not include medications they stopped taking 1-2 weeks ago in the list of medications they are taking. It is also important to consider the possibility of cross-allergic reactions, such as the combination of some diuretics (furosemide, thiazides) with sulfonamides, or penicillin with semi-synthetic antibiotics that differ from the original drug by side chains.
Allergic testing has limited reliability because the true allergen is often an unknown metabolite. Tests can give both false negative and false positive results. For example, after treatment with penicillin, hemagglutinating antibodies are often detected without evidence of a hemolytic process. Provocation testing with drugs carries the risk of severe allergic reactions, as fatal reactions can occur with very small doses of the suspected drug. Sublingual, intradermal, and intramuscular tests with gradual increases in drug dose can only be performed by an allergist in a hospital setting.
Skin prick tests are used only to detect delayed-type allergies. Their reliability is low because the cause of the hypersensitivity that develops is often not the drug itself but its metabolites.
Laboratory tests such as basophil degranulation, hemagglutination (agglutination of the patient's erythrocytes loaded with allergen serum), detection of precipitins, immunoglobulins IgE, IgG, IgM, leukocyte migration inhibition, lymphocyte blast transformation, and others can yield both false-positive and false-negative results. Laboratory diagnosis is further complicated by the fact that antigen-specific IgE can only be determined for a limited number of drug preparations. The absence of specific IgE to a drug does not rule out an allergic reaction to its administration.
Confirmation of the diagnosis of drug eruption is either the reduction or disappearance of symptoms after discontinuation of the suspected drug. This marker is also relative because eruptions may persist for a long time even after the drug has been discontinued.- Syphilitic roseola
- Pityriasis rosea
- Cat scratch disease
- Guttate psoriasis
- Lichen planus
- Ringworm
- Allergic contact dermatitis
- Eczema
- Erythema multiforme
- Rubella
- Scarlet fever
- Measles
- Viral exanthem
General Remarks on Therapy
- All medications should be discontinued except those that are vital and cannot be replaced by medications from another group.
- The amount of drug therapy depends on the severity of the disease, which is determined by the following criteria:
- The nature of the rash (localized or generalized).
- Tendency to erythroderma.
- Involvement of mucous membranes.
- Presence of hemorrhagic lesions.
- Presence of symptoms of general intoxication (general weakness, malaise, headache, dizziness, fever).
- Involvement of internal organs.
- Changes in complete blood count (elevated ESR, leukocytosis, anemia, thrombocytopenia).
Indications for hospitalization
- Widespread hemorrhagic and/or bullous lesions.
- Risk of developing severe forms of drug eruptions (Quincke's edema, Stevens-Johnson or Lyell syndrome).
- Persistent and widespread disease resistant to treatment.
- Presence of concomitant severe somatic diseases, fever, arthralgia, low blood pressure, lymphocytosis with atypical lymphocytes.
Systemic Therapy
Antihistamines are prescribed for predominant macular, urticarial, or papular eruptions:
- Cetirizine hydrochloride: for children aged over 6 years, 5 mg orally twice a day; for adults, 10 mg orally once a day for 7-10 days or
- Loratadine: for children aged 3 to 12 years and/or with a body weight less than 30 kg, 5 mg orally once a day for 7-10 days; for adults and children aged over 12 years and/or with a body weight of more than 30 kg, 10 mg orally once a day for 7-10 days or
- Chloropyramine: for children aged 1 year to 6 years, 8.3 mg orally 2-3 times a day for 7-10 days, for children aged 6 to 14 years, 12.5 mg orally 2-3 times a day for 7-10 days, for adults, 25 mg orally 3-4 times a day for 7-10 days or
- Clemastine: for children aged over 7 years, 0.5-1 mg orally twice a day for 7-10 days, for adults, 1 mg orally twice a day for 7-10 days
In severe cases of the disease, oral and/or parenteral glucocorticoids are prescribed. Dosages depend on the severity of clinical manifestations, but are not less than 30-35 mg per day in terms of prednisone.
Tactics in Case of Ineffective Treatment
In cases where macular, urticarial, or papular eruptions predominate, antihistamines may be substituted. If there is no effect even in this case, systemic glucocorticoids are prescribed orally and/or parenterally. The dosage depends on the severity of the clinical manifestations, but should not be less than 30-35 mg per day in terms of prednisolone.
Prevention
Prevention of recurrence of the disease involves informing the patient about the cause of the disease to eliminate this factor from their diet or from the approved pharmacological agents for use.