Scabies is a common parasitic skin disease caused by the scabies mite, Sarcoptes scabiei (L.). ICD-10 Code: B86
The causative agent is the scabies mite, Sarcoptes scabiei. Scabies mites are considered persistent parasites because they spend most of their life in the host's skin, with only brief periods of ectoparasitism on the skin surface.
The daily activity rhythm of the scabies mite explains the increased itchiness in the evening, the predominance of direct transmission during nocturnal bed contact, and the efficacy of nocturnal scabicide treatments.
A scabies outbreak is defined as a group of people that includes an infected individual who serves as a source of infection and provides conditions for transmission of the pathogen. The spread of the outbreak is influenced by contact with the infected person in bed during the night when the pathogen is most active (direct transmission). At least ten minutes of sufficient and continuous skin-to-skin contact is required for mites to be transmitted to another human host.
The second most important epidemiological setting is invasion-contact groups - groups of people who live together and share a common sleeping area (such as dormitories, children's homes, nursing homes, barracks, "supervisory" wards in psychiatric hospitals, etc.) with close household contacts during the evening and nighttime.
Classification:
- Classical scabies
- Scabies without burrows
- "Prurigo scabiosa" or "incognito" scabies.
- Nodular scabies.
- Erythrodermic Scabies.
- Norwegian scabies (Crusted scabies)
Classical scabies
Classical scabies is the most common and presents with various forms of scabies burrows, follicular papules on the trunk and limbs, non-inflammatory vesicles near the burrows, excoriations and bloody crusts distributed over the entire skin surface. It is characteristic of classic scabies that there are no eruptions in the interscapular region.
The eruptions are due to the activity of the mite (scabies burrows, follicular papules, non-inflammatory vesicles), the body's allergic reaction to its metabolic products (miliary papules, excoriations, bloody crusts) and pyogenic microflora (pustules).
Papules, vesicles, excoriations, and hemorrhagic crusts often dominate the clinical presentation of the disease. Papules with mites are characterized by a follicular arrangement and small size (up to 2 mm). Vesicles are typically small (up to 3 mm), without signs of inflammation, and are found primarily on the hands, less commonly on the wrists and feet.
Itching is a characteristic symptom of scabies caused by the body's sensitization to the parasite. Itching occurs 7-14 days after primary infection and within a day after reinfection. The intensification of itching in the evening and at night is associated with the circadian rhythm of parasite activity.
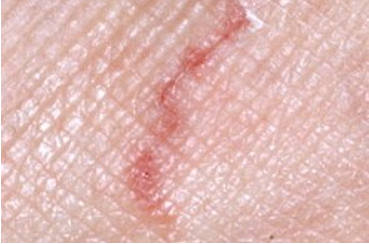
Scabies Burrows
Scabies burrows are the primary clinical symptom of scabies. Typical burrows appear as slightly raised lines of whitish or dirty gray color, straight or curved, 5-7 mm in length.
Burrows are found on the hands of almost all patients, and less commonly on the wrists, feet, and genitalia of males. The presence of scabies burrows on the feet is typical for patients with a long history of the disease, individuals in contact with petroleum products, and during the initial penetration of the female mite into the sole skin. This often occurs in baths and showers if they have been visited by people with a high parasitic index (the number of reproductive scabies burrows on an infected person) who had scabies.
Diagnostic signs of scabies
Scabies without Burrows
Scabies without burrows is less common than typical scabies and is primarily identified during the examination of individuals who have been in contact with scabies-infected individuals. It occurs upon infestation with larvae, exists in its initial form for no more than 2 weeks, and is clinically characterized by isolated follicular papules and non-inflammatory vesicles.
Prurigo scabiosa (scabies incognito)
Scabies of “clean people”
This occurs in people who frequently take water baths, especially in the evening, which washes off the female mites from the skin. Clinically, it corresponds to typical scabies with minimal manifestations.
Nodular scabies
Erythrodermic scabies
Bullous Scabies
Norwegian (Crusted) Scabies
Scabies in children
Diagnosis is established based on a complex of clinical and epidemiological data, confirmed by laboratory examinations aimed at detecting the causative agent.
Diagnosis should be confirmed by the detection of the causative agent.
- Staining method is used to verify scabies burrows. Suspicious elements resembling scabies burrows are smeared with an alcoholic solution of iodine or aniline dyes.
- Method of diascopy is based on visualizing superficial skin granules by depleting the capillaries when pressure is applied with a glass slide.
- Lactic acid diagnostic method involves applying 2-3 drops of a 40% lactic acid solution to a scabies burrow, papule, vesicle or crust. After 5 minutes, the loosened epidermis is vigorously scraped off with a scalpel. The material obtained is transferred to a microscope slide in a drop of the same lactic acid, covered with a coverslip and examined at low magnification. To accelerate the removal of epidermal scales, the slide may be gently heated over a burner flame. This method is convenient because lactic acid is used both as a substance that loosens the epidermis before scraping and prevents its dispersion, and as a substance that clears and fixes the material during microscopy. Lactic acid does not irritate the skin and its bactericidal properties prevent the development of pyogenic complications at the scraping sites. Unlike alkaline solutions, preparations in lactic acid do not crystallize, allowing them to be stored for long periods and used as teaching aids. This method is known for its speed and reliability in diagnosing scabies.
- Mineral Oil Scraping: A small drop of mineral oil (paraffin or petroleum jelly) is applied to the scabies lesion and scraped. Material from 5-6 scabies lesions, along with residual oil, is transferred to a microscope slide, covered with a coverslip, and examined at low magnification.
- Needle extraction method: This method is quick and effective if the doctor has good vision and sufficient skill to locate the burrow. Sterile needles are used. The needle is used to open the blind end of the burrow at the location of the brownish pinpoint elevation where the female scabies mite is located. The tip of the needle is used to cut the roof of the burrow around the mite, and then the needle is advanced along the direction of the burrow to extract the female, which attaches itself to the needle with its suckers. The mite is then placed on a slide and examined under a microscope at low magnification. This method is less suitable for detecting mites in old, disrupted burrows, papules, vesicles or after treatment with a scabicide. In cases of inadequate visual acuity, illuminated loupes or special head magnifiers are used.
- Thin section method: A piece of stratum corneum of the epidermis is cut from the scabies burrow or vesicle with a sharp sterile blade or ophthalmic scissors. After treatment with a 20% solution of sodium hydroxide (or potassium hydroxide) for 5 minutes, the material is examined under a microscope. Unlike the previous method, this method allows the detection of not only the mite, but also its eggs, shells, and excrement. This method requires good preparation and the availability of very sharp sterile instruments, which makes its widespread use difficult.
Laboratory diagnostic results are considered positive if microscopic examination of the specimen reveals a female, male, larva, nymph, egg, or empty egg shell. The presence of feces indicates the need for additional examination of another area of the skin.
Dermoscopy
Dermoscopy is a mandatory method when examining a patient with scabies. In cases of typical scabies, dermoscopy is positive in all cases, while in cases of scabies without burrows, it is positive in 1/3 of the cases. The detection of scabies burrows increases by one third compared to the examination of a patient without optical instruments. In cases of destroyed burrows and absence of female scabies mites in them, examination of externally unaltered skin near the burrow, covering an area of at least 4 cm2, is performed.
Dermoscopy reveals erosions, inflammation, and a small pigment triangle in the upper part of the burrow corresponding to the mite's mouthparts and anterior limbs. Depending on the position of the mite, the triangle is either completely (ventral projection) or partially (dorsal projection) visible.
- Mite Dermatitis
- Cercarial Dermatitis
- Atopic eczema
- Acropustulosis of infancy
- Arthropod Bites
- Contact Dermatitis
- Impetigo
- Eczema
- Langerhans Cell Histiocytosis (LCH)
- Papular Urticaria
- Psoriasis
- Seborrheic Dermatitis
- Viral Infections
- Pruritus
- Chickenpox
General Treatment Considerations
Treatment for scabies is categorized according to the physician's goals. There are three types of treatment:
- Specific treatment: This is administered when a patient has confirmed clinical and laboratory diagnosis of scabies through the detection of the causative agent.
- Prophylactic treatment: Administered based on epidemiologic evidence to individuals in scabies outbreak areas, even if they do not have clinical symptoms of the disease. This includes family members in affected households (parents, children, grandparents, other relatives), as well as caregivers and caretakers. It is applied when the conditions for transmission of the causative agent are present (close physical contact, sexual contact, sharing a bed in the evening and at night, etc.), or when several scabies cases are registered within a group/class/unit, or when new cases appear during surveillance.
- Trial treatment (ex juvantibus): This is conducted in cases where the physician suspects scabies based on clinical data but the diagnosis is not confirmed by the detection of the causative agent. If there is a positive response to scabicides, the case is registered as scabies.
The principles of therapy should be followed by the physician regardless of the scabicide chosen for scabies treatment:
- Treat all identified individuals in the outbreak simultaneously to prevent reinfection.
- Apply scabicides in the evening to enhance treatment effectiveness, considering the mite's nocturnal activity.
- For scabicides approved for use on children under 3 years of age, apply to the entire surface of the skin. For other patients, the face and scalp are exceptions.
- Apply scabicides with bare hands, not a cloth or swab. Be sure to thoroughly rub the product into the palms and soles of the hands.
- If hand washing is necessary after applying the scabicide, reapply the product to the hands.
- Perform a complete body wash before the first scabicide application and after completing the course of treatment. Change clothing and bedding after the course of treatment.
- Leave the scabicide on the skin for at least 12 hours, including the entire night. It can be washed off in the morning.
- Treat complications concurrently with scabies treatment.
- In cases of post-scabies pruritus, the question of retreatment with a scabicide is decided on an individual basis after a thorough examination of the patient.
- Disinfect clothing, bedding, towels, clothing, and shoes after treatment is complete. Perform wet cleaning in the room where the patient stayed.
Treatment regimens
Benzyl benzoate emulsion and ointment are preparations based on the benzyl ether of benzoic acid. A 10% emulsion and ointment are used for children 3 to 7 years old, while a 20% emulsion and benzyl benzoate ointment are used for the elderly. It is recommended that the patient wash with soap before starting treatment. Shake the emulsion before use. These preparations are applied to the skin twice - on the 1st and 4th day of treatment. The product can be washed off the skin after 12 hours of exposure. Change underwear and bedding on the 5th day. Burning sensation upon application to the skin is common and usually subsides within a few minutes, which should be explained to the patient. Avoid contact of benzyl benzoate with mucous membranes. Benzyl benzoate is contraindicated in pregnant women and children under 3 years of age.
Permethrin 5% Emulsion Concentrate in Ethanol. Prepare a 0.4% aqueous emulsion by diluting 8 ml of 5% permethrin emulsion concentrate with water at room temperature to a total volume of 100 ml. Apply to the skin once a day at night for 3 consecutive days or on the 1st and 4th day of the course. It is not recommended for use during lactation, in children under 1 year of age, and in elderly persons with liver or kidney failure.
Sulphur ointment is a preparation based on precipitated sulphur (33% sulphur). Apply Sulphur Ointment to the skin after washing with soap once a day at night for 5-7 days. Rub the product thoroughly into the skin of the hands, trunk, and legs, including the soles and toes. It is not recommended for use during pregnancy and in children under 3 years of age.
Piperonyl butoxide + esbiol aerosol for external use. After washing the patient, spray the product onto the skin from a distance of 20-30 cm. Start treating skin from the top of the body. For children's faces, apply the product with a cotton swab soaked in the product. After 12 hours, the patient should wash and change bedding and underwear. For uncomplicated scabies with no burrows and no complications, a single treatment is sufficient. For complicated scabies, repeat treatment in 3-5 days. Avoid contact of the medication with mucous membranes. This method is recommended for the treatment of scabies in patients with atopic dermatitis.
Treatment of pregnant women
For the treatment of scabies in pregnant women, caution should be exercised when using the external aerosol containing piperonyl butoxide + esbiol and the solution of permethrin prepared from a 5% emulsion concentrate in ethanol.
Treatment of children
For children under 1 year of age, an external aerosol containing piperonyl butoxide + esbiol is used. For children 1 to 3 years of age, use a topical aerosol containing piperonyl butoxide + esbiol and a 5% concentrate emulsion of permethrin in ethanol. For children aged 3-7 years, in addition to the above treatments, a 10% emulsion and benzyl benzoate ointment and 5% sulfur ointment are included in the therapy. Treatment of children older than 7 years is carried out according to the regimens used for adult patients.
Treatment of Nodular Scabies
After a full course of treatment with any scabicide, the mites will be eradicated. This process can be accelerated by gently scraping the epidermis from the surface of the papules with a sterile scalpel until small drops of blood appear before starting specific therapy. The skin defect is then treated with antiseptics (aniline dyes, 5% potassium permanganate solution, povidone-iodine solution, chlorhexidine digluconate, etc.).
Specific treatment with scabicides (in the evening) is combined with application of topical combination glucocorticosteroid preparations to papules (in the morning and during the day). These preparations include: diflucortolone + isoconazole, betamethasone + gentamicin + clotrimazole, hydrocortisone + neomycin + natamycin, clioquinol + flumetasone, and others.
If nodular scabies is observed after resolution of the primary clinical manifestations of scabies, treatment continues with single-component topical corticosteroids under occlusive dressings. These corticosteroids include methylprednisolone aceponate, hydrocortisone butyrate, mometasone furoate, and others. Superficial cryodestruction of lesions followed by application of topical combination glucocorticosteroids is also used.
Treatment of scabies complicated by allergic dermatitis
Before starting specific therapy, it is advisable to recommend washing with soap to improve access of the scabicide to the burrows. Treatment begins with the application of a scabicide to eliminate the activity of the scabies mite, which produces allergens. Preference is given to scabicides that do not require intensive rubbing and do not contribute to the spread of infection on the skin (topical aerosol containing piperonyl butoxide + esbiol and the solution of permethrin prepared from a 5% emulsion concentrate in ethanol). The scabicide is applied on the 1st and 4th day of the course, and the allergic dermatitis is treated on the 2nd and 3rd day.
For localized processes, only topical therapy is appropriate. For this purpose, combined topical glucocorticosteroid preparations are used, such as fluocortolone + isoconazole, betamethasone + gentamicin + clotrimazole, hydrocortisone + neomycin + natamycin, clioquinol + flumetasone, and others.
In case of widespread allergic dermatitis, it is necessary to prescribe oral antihistamines (levocetirizine, chloropyramine hydrochloride, clemastine, cetirizine, desloratadine, etc.). Topical therapy in this case begins with a shaken aqueous mixture, Zincol and other indifferent agents, including products for care of dry irritated skin. After the transformation of the widespread process into a localized one, the treatment can be continued with monocomponent topical glucocorticosteroids: methylprednisolone aceponate, hydrocortisone butyrate, mometasone furoate, and others.
Treatment of Norwegian Scabies
It has specific characteristics. In the evening, the patient is treated with a scabicide to eliminate active stages of the pathogen and reduce the patient's risk of infection. In the morning, one of the keratolytic agents is applied, such as products containing salicylic acid (5% sulfur-salicylic ointment, 5-10% salicylic ointment) and urea. This treatment is continued until the crusts are completely gone. Then the patient is treated with a scabicide only in the evening for 2-3 days.
After completion of specific therapy to eliminate dry skin, moisturizers or emollients are used. Regular examination of epidermal scrapings for scabies mites is essential. If mobile mites are found, the course of specific therapy is repeated with a change of scabicide.
Treatment of erythrodermic scabies
Treatment is similar to Norwegian scabies, but without the use of keratolytic agents.
Post-scabies pruritus
The persistence of pruritus in patients after complete specific therapy with one of the scabicides. The primary objective clinical symptom is the presence of scabetic burrows, the length of which can reach several centimeters. The absence of openings in the roof of such burrows hinders the penetration of the scabicide into them. The duration of pruritus corresponds to the life span of females and depends on their age at the start of treatment. If itching persists after one week of treatment with antihistamines and topical glucocorticosteroids (the time required for the epidermis to peel off the dead mites), a repeat scabicide treatment is necessary, performed after thoroughly washing the patient with soap and a washcloth. Another cause of itching may be dry skin. In this case, emollients are prescribed.
Treatment of scabies in hot weather
Preference is given to medications in liquid forms (topical aerosol with piperonyl butoxide and esbiothrin and permethrin solution prepared from 5% emulsion concentrate in ethanol), which do not require intensive rubbing. Use of ointments in high temperature conditions may result in overheating of the patient, development of dermatitis, or onset of bacterial infection.
Observation Periods
Observation periods for patients are individual and depend on their clinical form of scabies. In cases of scabies without burrows, classic scabies, "incognito" scabies after a full course of therapy and the implementation of a complete set of preventive measures in the focus, the observation period for patients is 2 weeks.
The duration of outpatient observation increases for scabies complicated by bacterial infection, dermatitis, nummular eczema, nodular scabies, erythrodermic scabies and Norwegian scabies. A patient is removed from the registry after complete resolution of all clinical manifestations. The prognosis for scabies is good.
Causes of Treatment Ineffectiveness
- Non-compliance with treatment regimens:
- Use of medications at lower concentrations
- Non-compliance with treatment frequency and timing.
- Application of the medication without considering the diurnal activity rhythm of the scabies mite.
- Partial treatment of the skin.
- Use of scabicides past their expiration date.
- Reinvasion in the absence or incomplete implementation of epidemiological control measures in the focus.
- Resistance of mites to scabicides.