Kaposi sarcoma is a disease associated with human herpesvirus 8 (HHV-8) characterized by multiple cutaneous and extracutaneous endothelial-derived neoplasms. ICD-10 codes: C46.0, B21.0.
Human herpesvirus 8 (HHV-8) belongs to the family g-herpesviridae, genus Rhadinovirus. Like other herpesviruses, HHV-8 gene expression is associated with viral latency or lytic viral replication.
The prevalence of classic Kaposi sarcoma varies widely among geographic regions, ranging from 0.14 per 1 million population (both men and women) to 10.5 per 1 million men and 2.7 per 1 million women. It is three times more common in men. Onset occurs between the ages of 35-39 in men and 25-39 in women.
One of the main routes of HHV-8 transmission is sexual, with an increased risk associated with the number of sexual partners and non-traditional sexual activities. The oral cavity is a site of significant viral replication, with high levels of HHV-8 copies present in saliva. Non-sexual transmission through saliva is widely recognized and is important for infecting children in endemic areas.
HHV-8 can also be transmitted through blood, blood products and donor organs after transplantation. The HHV-8 viral genome is detectable in all disease elements at all stages, regardless of clinical variants.
Classic Kaposi Sarcoma
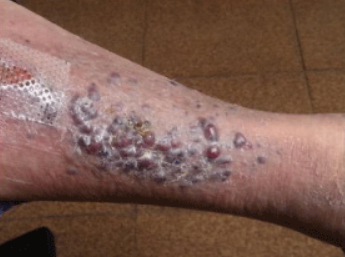
On the skin of the distal parts of the lower extremities, single or bilateral bluish-red patches, 1-5 cm in diameter, with well-defined borders, resembling hematomas, appear. These elements grow slowly, transforming into dense nodules (which coalesce to form plaques) and nodules. Large nodules on the lower extremities darken (due to hemosiderin deposition) and ulcerate, resulting in rejection of necrotic tissue. Pronounced edema with signs of lymphostasis is observed at the periphery of the nodules (subsequently forming fibrotic areas).
The classic form of Kaposi sarcoma usually follows a benign course with slow proximal spread. Patients may live for decades with slowly progressive disease. The spread of lesions to other areas of the body, lymph nodes, mucous membranes of the oral cavity and genitals, internal organs (often with asymptomatic progression) occurs within 2-3 years.
Fatal outcomes in the classical form are more often due to other causes, as the disease is observed in elderly individuals and develops slowly.
Endemic (African) Kaposi Sarcoma
AIDS-associated Kaposi sarcoma (epidemic type)
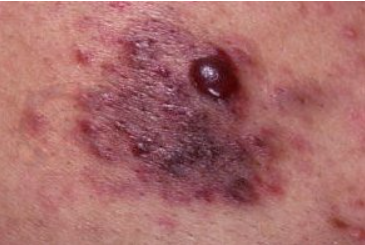
Characterized by rapid progression with multifocal spread. Primary facial manifestations are often seen on the skin of the nose, eyelids, ears, and trunk along lines of least skin tension. If left untreated, disseminated elements may coalesce into large plaques that spread to the skin of the face, trunk, or extremities, often leading to organ dysfunction. Oral mucosa is affected in 10-15% of patients. The most typical location for eruptions is the area of the hard and soft palate and the base of the tongue, where they rapidly ulcerate. Throat involvement is also common, leading to difficulty eating, speaking, and breathing.
The lymph nodes, gastrointestinal tract and lungs are also involved in the inflammatory process. The stomach and duodenum are favored sites of involvement, and the disease is often associated with bleeding and intestinal obstruction. In the pulmonary form, respiratory symptoms such as bronchospasm, cough, and progressive respiratory failure may occur.
Immunosuppressive Kaposi Sarcoma
- Hematoma
- Bacillary angiomatosis
- Pyogenic granuloma
- Angiosarcoma.
- Acroangiodermatitis
- Non-Hodgkin lymphoma
- Squamous cell carcinoma
Treatment Goals
- Reduce the severity of symptoms and prevent disease progression;
- Achieve tumor remission;
- Prolong the life and functionality of the patient;
- Improve the patient's quality of life.
General Treatment Considerations
Treatment options for Kaposi sarcoma depend on the clinical presentation of the disease, the size of the lesions, and the organs and/or systems involved in the pathologic process. Despite significant data suggesting that oncogenic herpesvirus infection caused by HHV-8 plays a central role in the pathogenesis of Kaposi sarcoma, the use of specific antiviral drugs is ineffective!
Treatment Methods
Localized form:
- Surgical excision
- Achieve tumor remission;
- Topical agents containing 9-cis-retinoic acid
- Radiation therapy
Disseminated forms (including internal organ involvement)
Treatment for Classic Kaposi Sarcoma
- Liposomal doxorubicin 20-40 mg/m2 every 2-4 weeks, 6-8 injections per course
- Vinblastine 6 mg IV once a week. Once response is achieved, a maintenance dose of 0.15 mg/kg is administered (every 7-14 days until symptoms are completely resolved).
- Doxorubicin/bleomycin/vincristine 20-30 mg/m2 /1-2 mg every 2-4 weeks until response is achieved
- Interferon-alpha 3-30 million IU daily intravenously for 3 weeks.
Treatment of AIDS-associated Kaposi's sarcoma
- Initiate highly active antiretroviral therapy. If ineffective, consider systemic cytostatic therapy.
Treatment for Patients Receiving Immunosuppressive Therapy
- Modify immunosuppressive regimen
- Liposomal doxorubicin 20-40 mg/m2 every 2-4 weeks, 6-8 injections per course
- Paclitaxel 100 mg/m2 every 2 weeks until response, monitor laboratory and functional parameters.