Gianotti-Crosti syndrome (Papular acrodermatitis of childhood) is a benign skin disorder in children characterized by symmetric papular eruptions on the limbs, face, buttocks, and occasionally the trunk. ICD-10 Code: L44.4.
Gianotti-Crosti syndrome is widely prevalent and occurs in children between the ages of 6 months and 14 years, with an average age of onset of about 2 years. The condition is more common in spring and early summer.
In the past, a distinction was made between true Gianotti-Crosti syndrome or papular acrodermatitis (as a manifestation of hepatitis B virus infection) and papulovesicular syndrome with acral localization (on the distal parts of the limbs), accompanying other viral infections or occurring in their absence. Currently, it is recognized that there are no differences between these two forms.
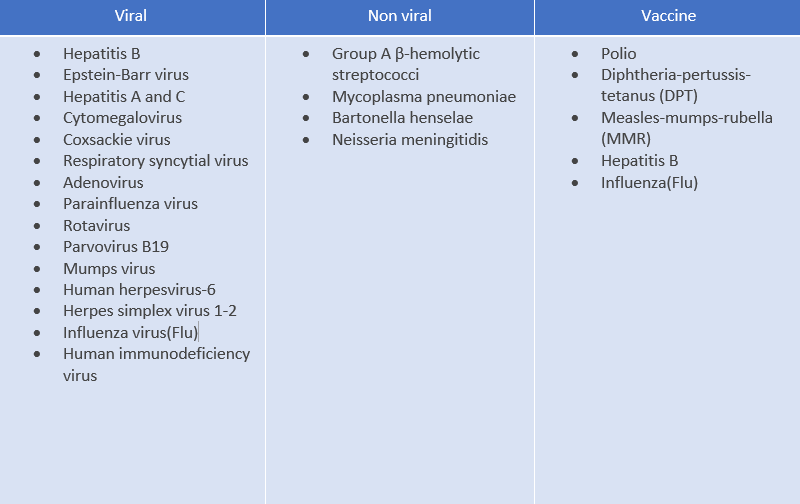
The condition is considered a self-limited cutaneous reaction to various infections. Although the exact pathogenesis is not fully understood, it is believed that immunization or immune imbalance increases the risk of developing the rash during or after infections. To date, the following infections have been identified as being associated with papular acral dermatitis in children:Gianotti-Crosti syndrome is usually preceded by a brief prodromal period characterized by subfebrile fever, weakness, and respiratory symptoms. This is followed by the sudden onset of a monomorphic symmetric papular eruption on the face, buttocks, and extensor surfaces of the limbs (including the palms and soles). The papules are typically lichenoid, 1-5 mm in size, and may be pink, dark red, or coppery in color. They are grouped but do not coalesce. Itching is often mild. In rare cases, the rash may spread to the trunk, and vesicles and purpura may appear.
In most cases, there is enlargement of the inguinal and axillary lymph nodes. Hepatomegaly and splenomegaly are common. The rash persists for 2 to 8 weeks (typically 3 weeks) and resolves spontaneously, while the hepatomegaly resolves later (within 2-3 months).
Atypical variants:
The diagnosis is based on a characteristic clinical presentation.
Diagnostic criteria (Chuh, 2001):
Confirmatory criteria:- Monomorphic, dome-shaped, pink-brown papules or papulo-vesicles measuring 1 to 10 mm in diameter.
- Involvement of any 3 or all 4 affected areas: face, buttocks, forearms, and extensor surfaces of the legs.
- Symmetrical rash.
- Duration for more than 10 days.
- Spread of the rash to the trunk.
- Scaling of the affected areas.
Laboratory tests:
To rule out viral hepatitis, serologic and molecular tests for hepatitis B virus are recommended, as well as blood biochemistry.
Histopathologic findings are nonspecific and include hyperkeratosis, acanthosis, focal spongiosis, vacuolar degeneration of the epidermis, perivascular lymphohistiocytic infiltrate in the dermis.- Lichen planus - Pruritus is more intense, with the most typical localization being the inner surface of the forearms. Facial involvement is rare. A reticular pattern called Wickham's striae (lace-like white lines) can be observed on the surface of larger papules and in the oral mucosa.
- Lichenoid drug eruption - History of medication intake, more intense pruritus, and a more diffuse nature of the disease.
- Papular urticaria - Severe pruritus, more urticarial papules, involvement of other family members, rapid improvement.
- Erythema multiforme - History of medication intake or herpes simplex virus, target-shaped lesions.
- Urticaria - severe pruritus, rapid change in the clinical presentation