Acropustulosis of infancy is a chronic and recurrent skin condition in early childhood characterized by a pruritic vesiculopustular rash on the extremities.
It affects children from a few months to 3 years of age, typically between 2 and 10 months, although cases have been reported at birth and at later ages. Etiology and pathogenesis are unclear. In most cases, the condition is associated with a previous scabies infection, but a definitive link has not been established. Some authors consider infantile acropustulosis to be a clinical variant of eosinophilic pustular folliculitis.The disease begins with a sudden onset of intensely pruritic erythematous papules, measuring 1-2 mm in diameter, which within 24 hours evolve into larger vesicles up to 4 mm, and then into pustules. Due to scratching, the pustules rupture, forming erosions that become covered with crusts. The appearance of new eruptions leads to a polymorphic presentation of papules, vesicles, pustules, erosions, and crusts.
After 7-10 days, the eruptions in most cases regress spontaneously, often leaving post-inflammatory macular hyperpigmentation. However, after 2-4 weeks, the disease relapses, especially during the summer months. The preferred sites for the rash are the soles, arches of the feet, palms, and occasionally the dorsum of the feet, fingers, toes, ankles, wrists, and forearms.
In very rare cases, the eruptions may spread to the trunk and face. Mucous membranes are usually not affected. Children are typically irritable, and their sleep is disturbed due to intense itching. The disease has a chronic course, with each new relapse having a shorter duration of eruptions, less intensity, and longer intervals between episodes. It usually lasts for several years and often resolves spontaneously by the age of 3-4 years.- Congenital syphilis
- Pustular psoriasis
- Pustulosis palmoplantar,pustular bacterid of Andrews
- Dyshidrotic eczema
- Langerhans cell histiocytosis
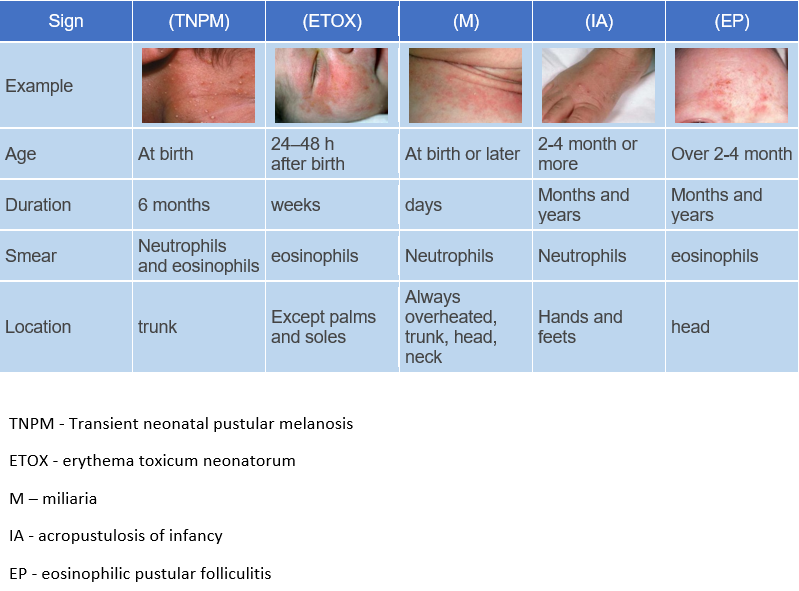
- Erythema toxicum neonatorum.
- It usually develops within the first 24-48 hours of life, but may be present at birth or appear after 10 days of age.
- It is characterized by the presence of erythematous macules of varying color, each with a papule, vesicle, or pustule at its center. Sometimes clusters of papules, vesicles, or pustules form erythematous plaques.
- The palms and soles are not involved in the pathological process.
- Individual lesions disappear within a few days of onset and the condition lasts a week or less.
- Hand, foot, and mouth disease
- Staphylococcal folliculitis.
- White or pale-yellow pustules with an erythematous halo.
- Microscopic examination of pustule reveals Staphylococcus aureus.
- Bullous impetigo.
- Flaccid blisters that rupture easily to form round or oval erosions covered with crusts; vesicles may also be observed.
- Microscopic examination of blister reveals Staphylococcus aureus.
- Scabies.
- Rarely seen in the first few months of life.
- Widespread rash; vesicles may be present, but red papules or nodules and burrows are more common.
- Microscopic examination of scrapings from papule surfaces obtained after application of mineral oil reveals mites, their eggs, and feces.
- Herpes simplex virus.
- Congenital candidiasis
- Widespread rash consisting of small, scaly, erythematous papules and pustules.
- Examination of scales or scrapings from papules treated with potassium hydroxide reveals pseudohyphae and fungal spores.
- Nail changes may be observed.
- Tinea (maanum and pedis)
- • Eosinophilic pustular folliculitis
- Papules and pustules typically located on the hairy part of the scalp.
- Has a chronic intermittent course.
Parents should be informed that the condition is self-limiting and that treatment should focus on relieving symptoms rather than curing the disease. Many authors recommend empirical treatment for scabies even if the scabies mite is not found in scrapings from the affected areas.
During a recurrence, the following are recommended:- Antihistamines: diphenhydramine at a dose of 1-1.25 mg/kg every 6 hours or hydroxyzine at a dose of 0.5 mg/kg every 12 hours and 1 mg/kg every 24 hours before bedtime.
- Topical corticosteroids: clobetasol propionate 0.05% or betamethasone dipropionate 0.05% ointment every 12 hours.
- Dapsone at a dose of 1-3 mg/kg.