Viral warts (verrucae) are benign proliferative skin and mucous membrane lesions caused by human papillomaviruses (HPV) and characterized by the development of epidermal growths. ICD-10 code: B07.
Viral warts are a fairly common pathology of the skin and mucous membranes in both children and adults. According to the observations of several authors, clinical manifestations of cutaneous HPV infection are observed in 3-9% of children and adolescents and in 28-30% of adults. There is no significant correlation between the frequency of this pathology and race or sex. Approximately 38-42% of individuals are carriers of HPV on apparently healthy skin.
The causative agent of the disease is the human papillomavirus (HPV), which belongs to the DNA-containing virus family Papavaviridae. To date, approximately 200 genotypes of HPV have been identified and characterized that infect humans, mammals, and birds. The genera that infect humans include alpha, beta, gamma, mu, and nu papillomaviruses. The most common causes of viral warts are HPV types 2, 27, and 57 (alpha papillomavirus), type 4 (gamma papillomavirus), and type 1 (mu papillomavirus). Less commonly detected are HPV types 3, 7, 10, and 28 (alpha papillomavirus), types 65, 88, and 95 (gamma papillomavirus), and type 41 (nu papillomavirus).
Human papillomaviruses have tissue specificity, the ability of certain HPV types to infect specific tissues associated with their localization:
- Types 1, 2, and 4 are detected in plantar warts.
- Types 2, 4, 26, 27, 29, and 57 are associated with common warts.
- Types 3, 10, 28, and 49 are found in flat warts.
- Types 2 and 7 are associated with butcher's warts
- Types 5, 8, 9, 10, 12, 15, 19, and 36 are associated with verruciform epidermodysplasia.
- Type 60 is associated with cystic warts.
Transmission of the virus can occur by direct or household contact, autoinoculation, or heteroinoculation at sites of epithelial tissue damage. The risk of HPV infection depends on several factors, such as the localization of the lesions, the viral load of HPV, the degree and type of contact, and the overall and local immune status. The presence of microtrauma and inflammatory processes in the skin may contribute to infection. It should be noted that HPV may be present not only in the basal layer of affected lesions but also in clinically intact adjacent skin and mucosa, where the virus may persist in a latent or low active state. Activation of the infection can lead to disease recurrence even several years after treatment. In the presence of favorable factors, the replication process of human papillomaviruses begins in the epithelium, leading to dysregulated cell differentiation and the formation of morphologically altered tissues.
There is no universally accepted classification.
Based on the characteristics of the clinical presentation of the disease, the following types of skin lesions are distinguished:
- Common warts
- Filiform warts
- Periungual warts
- Donut warts
- Palmoplantar warts
- Mosaic warts
- Subungual warts
- Cystic warts
- Flat warts
- Butcher's warts
- Focal epithelial hyperplasia (Heck's disease)
- Verruciform epidermodysplasia
Subjective symptoms of viral warts include:
- the presence of single or multiple papular formations on the skin and/or mucous membranes,
- tenderness upon compression in the areas where warts are located,
- deformations of the nail plates when growths form in the periungual area
- deformations of the foot in cases of extensive plantar skin involvement accompanied by significant pain.
Disease progression: Warts often disappear spontaneously over a period of several months to 5 years, especially in children. Warts in adults and patients with weakened immune systems may lead to complications such as erosions and, rarely, progression to squamous cell carcinoma. In immunocompetent individuals, warts almost never become malignant.
Common warts
Also known as verruca vulgaris. They are the most common condition caused by HPV, accounting for approximately 71% of all cases of cutaneous warts in humans. They often occur in children and adolescents, and the incubation period after viral inoculation can vary from several weeks to 18 months.
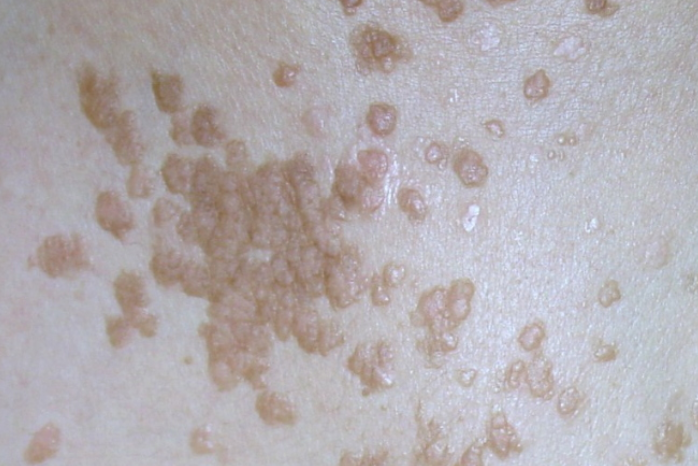
Common warts are characterized by multiple painless papules 0.2-0.5 cm in diameter. They have a color similar to normal skin and their surface is covered with cracks, keratinized layers, and papillomatous growths. They are most common on the backs of the hands, soles, fingers, around the nails, and on the knees. Secondary warts usually develop around the main "mother" wart. Common warts can also affect the oral cavity and the vermilion border of the lips.Filiform warts
Periungual Warts
Doughnut Warts
Plantar Warts
Plantar warts appear as dense, painful, rounded papules or plaques with a central depression and serrated or beveled edges. They have a color similar to the surrounding skin, are at the same level as the unaffected skin, and have a granular surface covered with hyperkeratotic layers. When the superficial layer is removed with a scalpel, black-brown dots of thrombosed capillaries are observed, and their disruption can cause bleeding.
On adjacent surfaces of the fingers, "kissing" warts can be found. Pressure on plantar warts usually causes pain.Mosaic Warts
Subungual Warts
Cystic Warts
Flat Warts
Also known as juvenile warts. They are less common (4%) and usually occur in children and adolescents. They are caused by HPV-3 and HPV-10 and tend to develop in areas of mechanical trauma, atopic dermatitis, and immunosuppression.
Clinically, flat warts appear as multiple flat papules with a polycyclic, round, or oval shape. In scratch areas, they may form linear lesions (Koebner phenomenon). They can be flesh-colored, yellowish, or reddish, have a smooth surface, and range in size from 1 to 3 mm, slightly raised (1-2 mm) above the skin level. They are commonly found in groups on the face (chin, forehead), back of the hands, forearms, shins, and occasionally on mucous membranes.Butcher's Warts
Focal Epithelial Hyperplasia (Heck Disease)
It is believed to be caused by a papillomavirus infection (HPV-1, 6, 11, 13, 32). It is considered a variant or stage of development of florid oral papillomatosis. It is more commonly observed in young individuals, particularly among Native Americans in North and South America, and cases have been reported in individuals with HIV infection.
Characteristic features include multiple flat hypertrophic papules and plaques of grayish-white color, ranging in size from 0.1 to 0.5 cm. They are scattered throughout the oral mucosa, predominantly in the areas of the cheeks, corners of the mouth, and vermilion border of the lips. When multiple lesions coalesce, the oral mucosa may resemble a "cobblestone pavement." Rarely, transformation to squamous cell carcinoma may occur.Epidermodysplasia Verruciformis
Common Warts:
- Molluscum Contagiousum is more commonly found on the trunk and genitalia and less commonly on the dorsum of the hands and feet. The lesions have a dome-shaped appearance with a central indentation, and when squeezed from the sides, a whitish, cheese-like material is expressed.
- Epidermal nevus, unlike common warts, is often solitary and typically exists from birth or early childhood. The nevus is significantly elevated above the skin surface, has a brown color, and is often covered with hair.
- Basal cell carcinoma typically develops in older individuals and has an infiltrative base. The periphery of the lesion has a typical peripheral rolled border composed of nodular elements (pearls), while the central part may have a crusted or ulcerated area that oozes slightly when the crust is removed..
- Granuloma annulare: Papules and nodules that typically form rings. Smooth surface.
- Knuckle pads (nodules in the area of interphalangeal joints): Plaques or papules above the interphalangeal joints. Smooth surface.
- A key diagnostic feature that distinguishes cutaneous verrucous tuberculosis from common warts is the marked inflammatory nature of the skin lesions in cutaneous tuberculosis verrucosa.
Plantar and Palmar Warts:
- Keratoderma of the palms and soles in Reiter's disease is characterized by larger size, conical shape, inflammation around the accumulated keratinized masses, and absence of black-brown thrombosed capillaries in the center of the lesion.
- Palmar and plantar syphilids are usually multiple, painless, and have a peripheral zone of desquamating epidermis. They are confirmed by positive serological tests for syphilis.
- Callus has a papillary pattern. Pressure on a wart in the direction of the skin fold often causes pain, whereas calluses are painful only when pressure is applied vertically. In addition, in plantar warts, the epithelium does not continue to the surface at the edges of the lesion, and when the superficial layer is removed with a scalpel, characteristic black dots (hemorrhagic capillaries of the papillary dermis) become visible..
Filiform Warts:
- Epidermal nevus with wart-like appearance.
- Skin tags
Flat Warts:
- Syringomas manifest as multiple papules, localized on the lower eyelid, inner corner of the eye, neck, and anterior chest wall. They are predominantly observed in women. Histologically, they show numerous cystic changes in the sweat gland ducts.
- Angiokeratoma of Mibelli presents with dark-red lesions, and histologically, there is marked dilation of capillaries.
- Unlike flat warts, papules of lichen planus are rarely located on the face. The eruptions in this condition are more widespread with umbilicated centers and a characteristic purplish hue. They have a "network" pattern (Wickham's striae) and histologically show irregular granulosis.
- Lichen Nitidus: Small, white or flesh-colored papules. There is often a history of atopy.
- Molluscum contagiosum: White or transparent papules, mainly with umbilicated centers.
- Benign histiocytosis with CNS involvement: Closely resembles flat warts. It is almost always localized on the face, with other areas of the skin being rarely affected.
Butcher's Warts
- Cutaneous Tuberculosis (Warty Tuberculosis)
Periungual Warts
- Periungual Calluses
- Acquired Digital Fibrokeratoma
- Bowen's Disease (Squamous Cell Carcinoma in Situ)
- Squamous Cell Carcinoma
- Tuberculosis
- Epidermal Nevus
- Lichen Planus
- Foreign Body Granuloma
Subungual Warts
- Bowen's Disease
- Squamous Cell Carcinoma
- Acquired Digital Fibrokeratoma
- Glomus Tumor
- Subungual Fibroma
- Foreign Body Granuloma
- Onychoclasia (Subungual Horn)
- Onychomatricoma
- Exostosis
- Enchondroma
Treatment goals:
- Destruction of viral warts
- Improvement of patients' quality of life
Indications for treatment include the presence of clinical manifestations of viral warts. Destructive therapy is the leading approach in the treatment of viral warts, despite its effectiveness ranging from 50% to 80% and the high likelihood of recurrence after tissue regeneration. There is a high risk of recurrence with extensive warts (covering an area greater than 2 cm2), plantar warts, and warts in the periungual area. The choice of treatment should be based on the location and extent of the affected areas.
Treatment for children: Preferred treatment methods for warts in children involve physical methods that do not cause toxic side effects.
Treatment outcome expectations: Clinical recovery.
Physical Methods:
- Electrocautery: Viral warts are removed layer by layer with electrocautery. Performed under local anesthesia with 2% lidocaine solution.
- Cryotherapy: Lesions are frozen using liquid nitrogen, nitrous oxide, or carbon dioxide.
- Laser Destruction: Warts are removed layer by layer using a laser. Performed under local anesthesia with 2% lidocaine solution.
- Radiofrequency Surgical Destruction: This method is based on the generation of electromagnetic waves of various frequencies ranging from 100 kHz to 105 MHz. Performed under local anesthesia with 2% lidocaine solution.
Alternative Methods:
- Collomak (salicylic acid + lactic acid):
- One or two drops should be applied to the affected areas 1-2 times a day.
- In adults, daily dose should not exceed 2.0 g of salicylic acid, which is approximately equivalent to 10.0 ml of Collomak solution. In children, daily dose should not exceed 0.2 g of salicylic acid, which is approximately equivalent to 1.0 ml of Collomak solution. When using this medication in children, multiple areas of the skin should not be treated simultaneously.
- Duration of treatment: When using the maximum daily dose (10.0 ml in adults and 1.0 ml in children), duration of treatment should not exceed 1 week. In case of multiple lesions on the skin, treatment with Collomak should be done in several stages with intervals.
- During this procedure, moderate redness and rarely swelling may occur on the healthy skin surrounding the application site, which will disappear completely within 24-48 hours after the procedure. These phenomena are considered normal, and no additional therapeutic measures are required. In case of pain, the treatment should be discontinued.
- Within a few days, treated area will turn dark brown color and form a scab. If the result is unsatisfactory, this procedure can be repeated after a few days. The scab should not be removed; it should fall off by itself (otherwise tissue healing may be compromised).
- Salicylic acid (plaster, solution, ointment):
- Application of 17% salicylic acid to the wart(s). Salicylic acid plaster can also be used.
- A higher concentration of salicylic acid may be used to treat plantar warts. Plasters with 40% salicylic acid are left on for 24-48 hours and then replaced. Treatment may last 6-8 weeks.
- After applying acid solution, surface is left to dry in the air for 2-3 minutes until a white memrane forms.
- Wart is covered with adhesive tape or any other occlusive dressing.
- Dressing is removed the next morning.
- If necessary, any remaining wart tissue can be gently removed with an emery board.
- Repeat application every evening until wart disappears.
- Notes:
- This method is most effective for plantar warts.
- Salicylic acid is not applied to the face, skin folds, or genital areas.
- If maceration or inflammation occurs, the treatment is discontinued for 1-3 days and then resumed.
- It may take up to 8 weeks for warts to disappear.
- Topical Retinoids:
- Since cryotherapy of flat warts in the facial area often leads to residual hypopigmentation, it is better to treat them with topical retinoids (cream with tretinoin, retinoic acid ointment).
- Cream with tretinoin 0.025%, 0.05%, or 0.1% is applied at night to the entire affected area. The frequency of application is adjusted to achieve mild peeling and erythema. Treatment can take several weeks to months.
- Significant improvement can be achieved with 5% fluorouracil cream when applied twice daily for 3-5 weeks. However, use of fluorouracil may cause persistent hyperpigmentation, which can be minimized by applying the cream directly to the affected areas using an applicator with a cotton tip.
- Imiquimod cream 5% is an immune response modulator with limited use in the treatment of common warts, as its effectiveness is limited by poor penetration into the skin.
- For common warts, treatment with liquid nitrogen is performed, followed by application of salicylic acid 17% at night and imiquimod in the morning under occlusion. The treatment is continued for 6-9 weeks. According to some reports, the effectiveness ranges from 50% to 100%.
- For flat warts, Imiquimod cream 5% is applied to the affected areas at night daily. If irritation is severe, the frequency of application may be reduced. Treatment may take several weeks.
- Cimetidine (30-40 mg/kg/day in divided doses for 6-8 weeks or longer) is effective in some cases.
Injections into warts:
- Bleomycin 0.5 IU/mL is injected into the wart for depigmentation. The number of injections depends on the size of the lesion. Warts that respond to treatment are covered with a hemorrhagic crust that heals without leaving scars. Treatment is very painful and may cause necrosis or severe vasospasm. It is contraindicated during pregnancy.
- Local immunotherapy with squaric acid (3,4-dihydroxy-3-cyclobutene-1,2-dione).
- Monochloroacetic acid (40% solution, plaster).
Treatment of flat facial warts in children with glycolic and salicylic acids:
A gel containing 15% glycolic acid and 2% salicylic acid was used for treatment. The gel was applied to the affected areas in a thin and even layer once a day in 20 patients aged 7 to 16 years. Complete healing was observed in 7 patients within 4 weeks and in 13 patients within 8 weeks. Temporary skin irritation was reported by 4 patients, and the gel was applied every other day until the symptoms resolved.
The proposed mechanism of action of the composition involves exfoliation and disappearance of corneocytes in the stratum corneum.
Treatment of plantar warts with hot water:
Foot baths are used for 30-45 minutes, 2-3 times a week, with the water temperature maintained at 43-45 degrees Celsius. The key aspect of the method is to maintain a constant water temperature. The effectiveness of local hyperthermia was demonstrated by Chinese researchers in a randomized clinical trial conducted in 2010 on 60 patients with plantar warts. The patients were divided into two groups: one group received hyperthermia and red light using a special device (44°C for 30 minutes, three consecutive days), and a placebo group received only red light. Healing occurred in 54% of the treated patients compared to 12% in the placebo group.
Systemic treatment:
Oral zinc sulphate 10 mg/kg daily