Vitiligo is a chronic condition of unknown etiology characterized by the appearance of depigmented patches and discolored hair on various parts of the body due to the destruction and reduction of melanocytes in the skin. ICD-10 code: L80.
The etiology of vitiligo is not yet understood. Several hypotheses regarding the pathogenesis of the disease include genetic, autoimmune, neurohumoral, oxidative stress, auto-cytotoxic, and convergent mechanisms. According to most experts, autoimmune mechanisms play a significant role in damaging melanocytes and disrupting melanogenesis processes in the skin of vitiligo patients. The prevalence of vitiligo in population ranges from 0.5% to 2%; the prevalence of the disease among children and adolescents does not differ from that among adults.
Based on the clinical presentation, the following types of vitiligo are distinguished:
Non-segmental Vitiligo:- Generalized vitiligo
- Acrofacial vitiligo
- Universal vitiligo
- Mixed vitiligo (combination of non-segmental and segmental vitiligo)
- Mucosal vitiligo (presence of multiple foci of involvement)
- Unisegmental vitiligo
- Bisegmental vitiligo
- Plurisegmental vitiligo
- Focal vitiligo
- Mucosal vitiligo (presence of a single focus of involvement)
Typically, single or multiple milky-white depigmented patches of various shapes and sizes with clear margins appear on the skin and, less commonly, on mucous membranes. These patches often appear at sites of skin trauma (Koebner's phenomenon) and tend to grow and coalesce peripherally. Residual pigmentation and, less commonly, hyperpigmentation of the skin, especially at the periphery of the lesions, may be observed in the depigmented areas.
Vitiligo patches typically develop on the skin of the eyelids, periorbital areas, neck, armpits, trunk, elbow joints, forearms, dorsum of the hands, genitals, perineum, knee and ankle joints, shins, and soles. Occasionally, they may be associated with one or more halo nevi (melanocytic nevi with a depigmented halo). Some patients may have discolored hair in the affected areas (eyelashes, eyebrows, scalp, axillary folds, pubic area, and other body regions). In rare cases, the appearance of white patches may be accompanied by itching, erythema and skin scaling.
The diagnosis of vitiligo is based on the patient's medical history and the clinical presentation of the disease, which includes the presence of milk-white patches with clear borders and typical localization on the skin. During the initial examination, it is advisable to document the appearance and location of the white patches through photography. For a more precise visualization of vitiligo lesions and to perform differential diagnosis, examination with a Wood's lamp is recommended.
Laboratory tests may include:
- Complete blood count
- Urinalysis
- Biochemical blood analysis (to determine glucose levels and assess liver and kidney function)
- Anti-thyroid peroxidase (TPO) antibodies and Anti-thyroglobulin (TG) antibodies
- Additional testing of other antibodies, such as antinuclear antibodies, antibodies against gastric parietal cells, etc., may be conducted to detect any associated autoimmune disorders.
- Histological examination of skin biopsies is indicated in cases where the diagnosis is unclear, and it is clinically difficult to determine the type of skin dyschromia.
- To rule out associated conditions, including other autoimmune diseases, it is recommended to seek consultation with a general practitioner (pediatrician), endocrinologist, otolaryngologist, gynecologist, ophthalmologist. Referral to other specialists may be warranted based on specific indications.
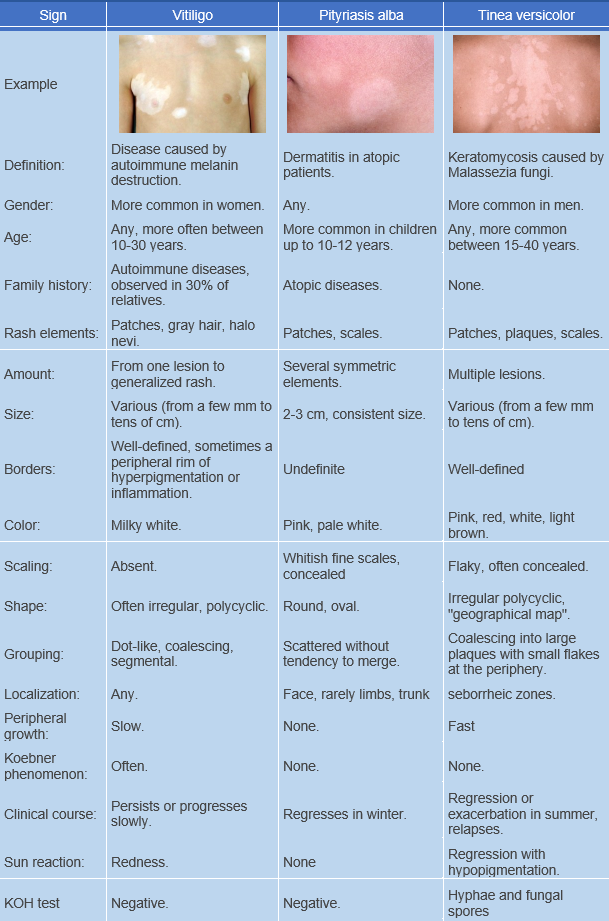
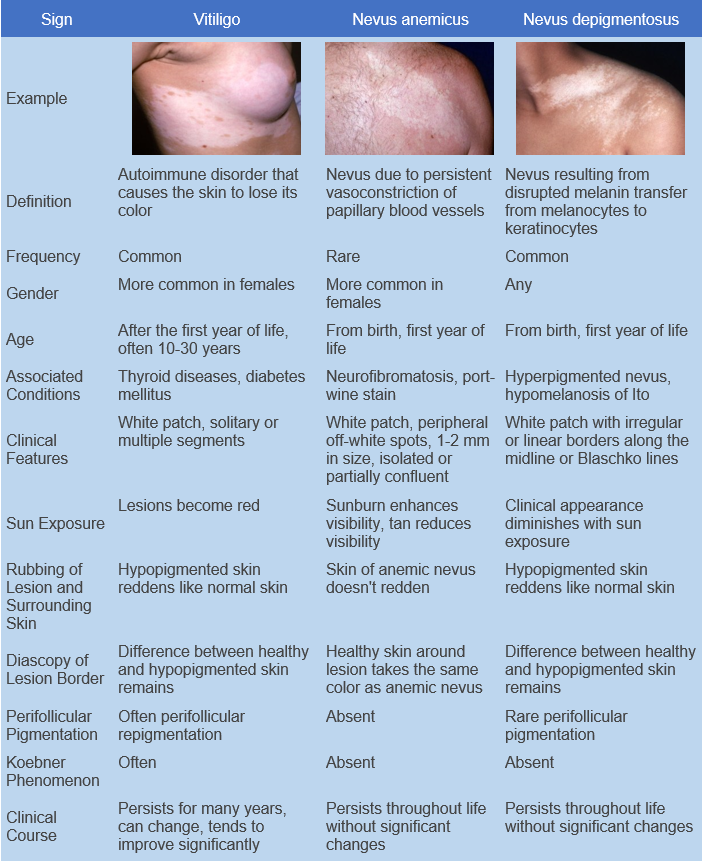
Vitiligo is commonly differentially diagnosed from the following conditions:
- Pityriasis versicolor (Tinea versicolor)
- Nevus depigmentosus
- Nevus Anemicus
- Lichen sclerosus
- Pityriasis alba
- Idiopathic guttate hypomelanosis
- Secondary leukoderma, which can develop with atopic dermatitis
- Syphilis
- Systemic lupus erythematosus
- Leprosy
- Pinta
Less frequently, vitiligo is differentiated from the following conditions:
- Piebaldism
- Albinism
- Vogt-Koyanagi-Harada syndrome
- Bloch-Sulzberger syndrome (Incontinentia pigmenti)
- Waardenburg syndrome
- Wolf syndrome
- Ito hypomelanosis
- Tuberous sclerosis
- Depigmentation induced by trauma or chemicals.
The goals are:
- To stop progression of the disease.
- To reduce activity of the pathological process.
- Repigmentation
- To improve the quality of life of the patients.
General Treatment Considerations:
- For limited forms of non-segmental vitiligo and segmental vitiligo, topical medications are the preferred treatment. If there is no response to topical treatments, medium wave ultraviolet therapy or ultraviolet excimer light with a wavelength of 308 nm may be used.
- For patients with widespread forms of vitiligo, narrowband phototherapy with a wavelength of 311 nm or broadband ultraviolet medium-wave therapy with a wavelength of 280-320 nm are the treatment of choice.
- For patients aged 18 and older who do not respond to other therapeutic approaches, PUVA therapy (Psoralen + UVA therapy) with oral administration of a photosensitizer is recommended.
- The maximum number of phototherapy and PUVA therapy sessions for the treatment of vitiligo has not been established. Considering the increased risk of skin cancer with multiple courses of PUVA therapy in psoriasis patients and the theoretical risk of carcinogenic effects of large cumulative doses of medium-wave ultraviolet radiation, patients with vitiligo and skin phototypes I-III should not undergo more than 150 PUVA therapy sessions and 200 narrowband phototherapy sessions with a wavelength of 311 nm throughout their lifetime.
- Treatment with topical corticosteroids, topical calcineurin inhibitors, and phototherapy is generally ineffective in patients with universal vitiligo.
- Patients should be informed of the extended duration of therapy, which may range from 6 months to 1 year or more.
Topical treatment:
Topical Glucocorticosteroids:
- Methylprednisolone aceponate, cream, or ointment, applied topically once daily as applications.
- Alclometasone dipropionate, cream, or ointment, applied topically once daily as applications.
- Betamethasone dipropionate, cream, or ointment, applied topically once daily as applications.
- Clobetasol propionate, cream, or ointment, applied topically once daily as applications.
Topical glucocorticosteroid preparations are the first-line therapy for patients with limited forms of non-segmental vitiligo and those with segmental vitiligo. Literature data indicate a moderate efficacy of vitiligo treatment with topical glucocorticosteroids.
Treatment with topical glucocorticosteroids can be carried out using continuous or intermittent methods.
In the continuous method, glucocorticosteroid preparations of moderate or high potency are prescribed for children and preparations of high or very high potency for adults, applied once daily for a maximum of 2-3 months. Continuous use of glucocorticosteroids is not recommended for facial lesions.
The intermittent method, using high or very high potency preparations, is preferable. Applications are made once daily for 2 weeks, followed by a 2-week break. If there are no side effects, 4-6 repeated courses can be performed.
Prolonged use of topical glucocorticosteroid preparations should be carried out with caution due to the possibility of developing local side effects (steroid acne, skin atrophy, stretch marks, hirsutism, infectious complications).
Topical Calcineurin Inhibitors:
- Tacrolimus 0.1% ointment, applied topically twice daily as applications.
- Tacrolimus 0.03% ointment, applied topically twice daily as applications.
- Pimecrolimus 1% cream, applied topically twice daily as applications.
For patients with limited forms of vitiligo for whom topical glucocorticosteroids have been ineffective, topical calcineurin inhibitors may be used as an alternative treatment. Several randomized, including placebo-controlled, trials have demonstrated the efficacy of 0.1% tacrolimus ointment in both adults and children with vitiligo. When comparing the results of vitiligo therapy in children using 0.1% tacrolimus ointment and clobetasol propionate preparations, no statistically significant differences were found. Positive effects were also observed in children treated with 0.03% tacrolimus ointment. The efficacy of 1% pimecrolimus cream in the treatment of vitiligo has also been demonstrated. Satisfactory effects are mainly observed in lesions localized on the face.
Treatment with topical calcineurin inhibitors lasts for 3 months or longer.
Topical calcineurin inhibitors are considered safer than topical glucocorticosteroids because they do not cause skin atrophy. It is not recommended to combine treatment with topical calcineurin inhibitors with phototherapy or sun exposure as this may increase the risk of developing skin tumors. Note: The instructions for use of Tacrolimus Ointment and Pimecrolimus Cream do not include vitiligo as an approved indication.
Analogs of vitamin D, such as topical calcipotriol, used in combination with phototherapy, can reduce the time to repigmentation and the overall accumulated photodose.
Oral treatment
- In progressive vitiligo, oral minipulse corticosteroid therapy (OMP) may be used to promote disease stabilization through immunosuppression. A typical regimen includes low-dose oral betamethasone or dexamethasone taken on 2 consecutive days per week for 3 to 6 months. Lack of disease stabilization after 3 months of combination therapy (OMP plus NB-UVB phototherapy) warrants discontinuation of the OMP only and reevaluation at 3-month intervals. Alternatively, upon failure of OMP, daily dosing with 20 mg of oral prednisone may be considered until disease progression has halted.
- Minocycline 100 mg/day for 4 weeks, through its anti-inflammatory, immunomodulatory, antioxidant, direct free radical scavenging, and anti-apoptotic properties, may be an effective therapy to arrest progression of vitiligo as well as induce repigmentation.
- Use of methotrexate, an immunomodulating systemic agent, has been shown to improve vitiligo in 1 of 3 patients with rapidly progressive, generalized vitiligo when administered in an uptitrating dose of 12.5-25 mg per week, as reported in a recently published case series. Repigmentation was noted as early as 6 weeks to 14 months in this patient, who had previously failed to respond to topical calcineurin inhibitors and phototherapy.
The role of antioxidants in the treatment of vitiligo remains controversial. Based on a systematic review of the literature performed by Speeckaert et al, the oxidative stress pathway is deregulated in patients with vitiligo, although this is not considered disease specific, but rather consistent with findings expected in an immune-mediated skin disorder. It has also been suggested that increased oxidative stress in non-lesional skin may be specific to vitiligo.
Among antioxidant therapies, oral Polypodium leucotomos (PL) extract has been studied in patients with generalized vitiligo due to its remarkable antioxidant and immunomodulatory properties. Oral Polypodium leucotomos 250 mg thrice daily with PUVA could show results in 4-6 months.
Ginkgo biloba extract has been shown to have some antioxidant and anti-inflammatory properties and may help induce stabilization of vitiligo. Ginkgo biloba extract 60 mg twice daily for 4-6 months could improve total Vitiligo Area Scoring Index measurements.
Light therapy
A randomized trial demonstrated the efficacy of NB-UVB monotherapy in vitiligo patients: after 6 months of treatment, the repigmentation rate in vitiligo patches was 42.9% compared to 3.3% in control areas (A) [15]. Patients with non-segmental vitiligo showed higher efficacy with NB-UVB compared to PUVA therapy (A) [16]. Treatment starts with a dose of 0.1-0.25 J/cm2 and sessions are performed 2-3 times per week (but not on consecutive days). At each subsequent session, the dose is increased by 5-20% until mild or moderate erythema, not accompanied by pruritus or pain. Once erythema is present, the dose is kept constant and if no erythema occurs, the dose is increased by 5-20%. The course of treatment includes 20 to 100 or more sessions.