Pyoderma gangrenosum is a reactive dermatosis characterized by chronic, non-infectious necrotic skin lesions that usually occur in association with a systemic condition. ICD-10 code: L88
Pyoderma gangrenosum is rare and affects men and women equally. The peak incidence is in the 25-54 year age group. Although rare, the condition may occur in children.
The exact etiology and pathogenesis are mostly unknown, but it is believed to be a manifestation of altered immune reactivity, as evidenced by numerous humoral and cell-mediated abnormalities observed in association with pyoderma gangrenosum.
The pathogenic response, which leads to the development of lesions at sites of trauma, represents an altered and uncontrolled inflammatory process observed in patients with immune reactivity disorders. Pyoderma gangrenosum is a neutrophilic dermatosis, histologically characterized by an intense dermal neutrophilic infiltrate without primary vasculitis.
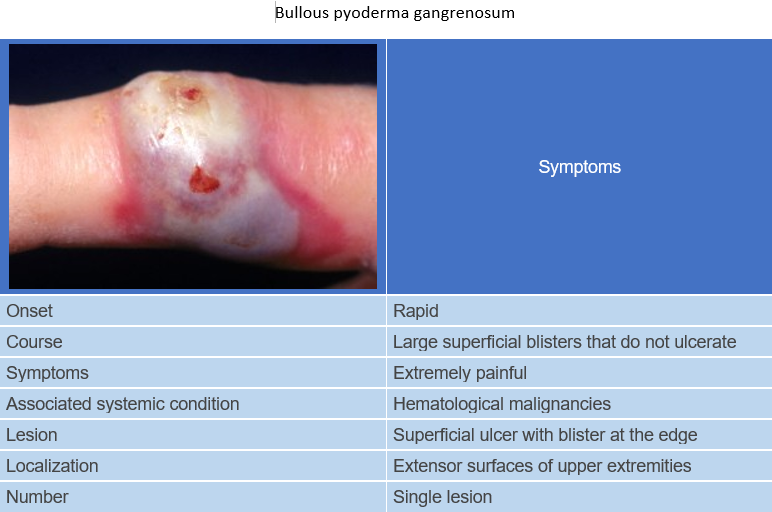
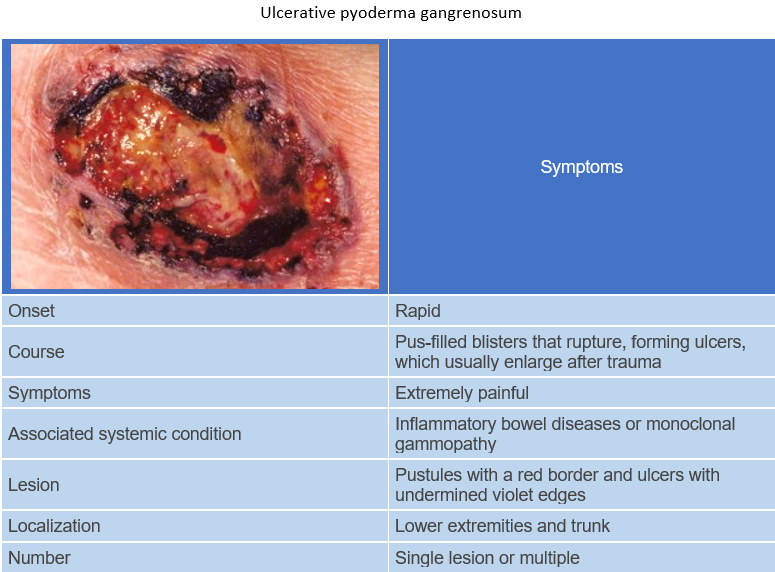
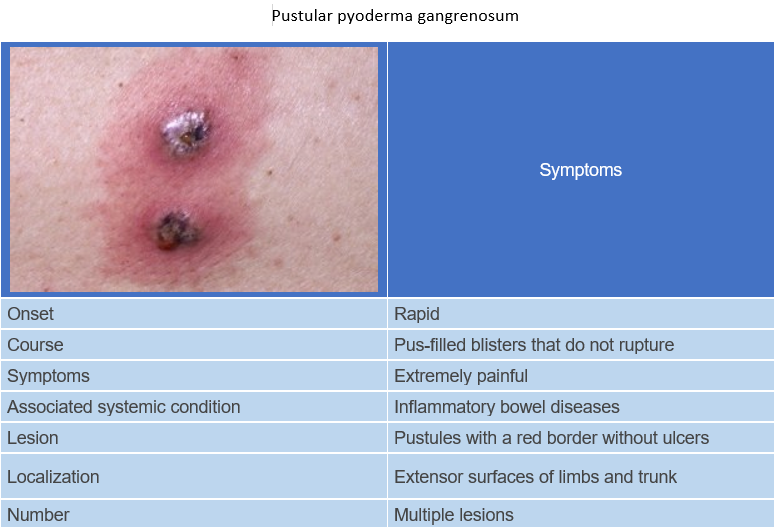
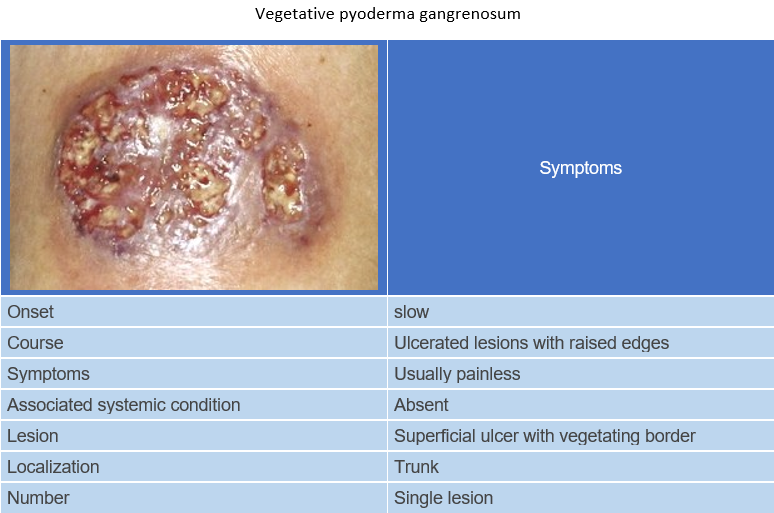
Clinically, pyoderma gangrenosum is classified into four forms:
- Ulcerative
- Pustular
- Bullous
- Vegetative
Systemic diseases that could be associated with pyoderma gangrenosum:
- Inflammatory bowel disease: Pyoderma gangrenosum is seen with equal frequency (1.5-5%) in both ulcerative colitis and Crohn's disease. It may precede, coexist with, or follow these diseases. It usually presents in an ulcerative or pustular form.
- Arthritis: 37% of cases of the ulcerative form are associated with arthritis. It is usually seronegative monoarthritis of the large joints and less commonly arthritis associated with inflammatory bowel disease, rheumatoid arthritis, Felty syndrome, osteoarthritis, and sacroiliitis.
- Immunologic disorders: Conditions such as congenital and acquired hypogammaglobulinemia, selective IgA deficiency, hyper-IgE syndrome, and immunosuppression may be associated with pyoderma gangrenosum.
- Monoclonal gammopathy: Occurs in 10% of cases, usually in the ulcerative form. Often associated with IgA secretion.
- Malignancies: In 7% of cases, pyoderma gangrenosum is associated with hematological malignancies, such as acute myeloid leukemia, chronic myeloid leukemia, multiple myeloma (IgA type), and Waldenström macroglobulinemia, as well as with solid tumors (rarely), including carcinoid, colorectal, bladder, prostate, breast, bronchial, or ovarian cancers.
- Other conditions: hepatitis, thyroid disease, possibly related to propylthiouracil treatment, autoimmune hemolytic anemia, chronic obstructive pulmonary disease, hidradenitis suppurativa, conglobate acne, sarcoidosis, atrophic gastritis, diabetes mellitus, systemic lupus erythematosus (SLE), and Takayasu's arteritis, among others.
The diagnosis is mainly based on clinical features since there are no pathognomonic histopathological characteristics or specific serological and hematological markers. It is a diagnosis of exclusion, and most tests are performed to rule out other conditions that may clinically resemble pyoderma gangrenosum.
Diagnostic criteria include:
- Development of painful ulcerative lesions following minor traumas.
- Severe pain in the affected area, which is not related to the depth of the lesion.
- Absence of pathogenic flora growth in bacterial culture tests.
Additional criteria include:
- Characteristic histopathological changes in the perilesional zone (abundant neutrophilic infiltration with signs of vasculitis, deposition of immunoglobulin G and complement in the dermal vessels).
- Frequent associations with conditions such as ulcerative colitis, Crohn's disease, rheumatoid arthritis, and blood disorders.
- Positive pathergy test (25-50%).
- Lack of response or poor response to traditional ulcer treatments.
- Positive response to systemic immunosuppressive therapy, showing active positive dynamics.
Tests to rule out conditions mimicking the disease include:
- Skin biopsy with hematoxylin and eosin staining, bacterial culture (bacteria, fungi, and mycobacteria), and direct immunofluorescence to rule out vasculitis.
- Blood tests: iodide and bromide; calcium and phosphate; lupus anticoagulant/anticardiolipin antibodies; antineutrophil cytoplasmic antibodies (C and P-ANCA); serological tests for syphilis.
Tests for the diagnosis of associated systemic diseases include:
- Gastrointestinal investigations: proctosigmoidoscopy/colonoscopy.
- Hematological tests: complete blood count, serum protein; Bence-Jones protein in urine; bone marrow biopsy; CT of chest/abdomen/pelvis and lymph node biopsy.
- Other tests: joint radiography, rheumatoid factor, antinuclear antibody; alpha-globulin and HIV.
- Tuberculosis and atypical mycobacterial infections
- Bacterial infections such as furuncle, ecthyma
- Syphilis
- Synergistic gangrene
- Blastomycosis-like pyoderma.
- Deep fungal infections
- Amoebiasis.
- Chronic herpes zoster virus infection in immunodeficient patients.
- Systemic vasculitis.
- Antiphospholipid syndrome.
- Necrotic arachnidism (spider bite).
- Primary malignant skin tumors.
- Metastases.
- Halogenoderma - iodides or bromides.
- Granulocyte-colony-stimulating factor (G-CSF).
- Isotretinoin.
- Trauma - including mechanical dermatoses.
- Calciphylaxis.
General Treatment Recommendations: Pyoderma gangrenosum is a rare disease, and as such, none of the recommended therapeutic modalities have been studied in large, randomized, placebo-controlled trials. Most evidence for the efficacy of these therapeutic agents is based on limited nonrandomized studies and individual reports. It is important to treat the underlying systemic disease, as most of these are serious and require treatment. In addition, treatment of any associated gastrointestinal disease leads to resolution of skin lesions.
Wound care: The primary goal of wound care is to create optimal conditions for re-epithelialization and closure, while controlling the inflammation that leads to ulceration.
The following measures are taken:
- Prevention and treatment of secondary wound infections, including daily wound cleansing with sterile saline and antiseptic solutions, hermetic hydrocolloid dressings that protect the wound and provide an acidic environment to inhibit microbial growth, continuous wound monitoring to exclude infection by obtaining wound surface fluid cultures, and immediate application of topical and systemic antibiotics at the first sign of infection.
- Wound bed debridement: Aggressive surgical debridement is contraindicated because of the pathergic reaction. Gentle debridement is therefore required, often achieved with moist saline dressings, 0.5% silver nitrate, Burrow's solution, potassium permanganate solution, as well as hydro-massage, hydrocolloid dressings or hydroactive gels. Facilitate re-epithelialization and wound closure: In addition to protecting the wound from infection, attempts can be made to stimulate wound reepithelialization by increasing the level of growth factors on the wound surface. This can be achieved with hermetic hydrocolloid dressings that concentrate growth factors at the wound surface, cultured keratinocyte autografts and split-thickness skin grafts with concomitant specific immunotherapy, and the use of topical growth factor preparations.
- A recent study reported that the use of bioengineered skin as an adjunct to cyclosporine immunosuppressive therapy accelerated healing and reduced pain in rapidly spreading leg ulcers. Within 2 weeks, the ulcer healed by 30-40%, and 100% re-epithelialization was achieved within 6 weeks.
Pain Management: Pyoderma gangrenosum (PG) lesions are very painful, and although specific therapy may relieve pain, immediate pain management measures are often required. These measures typically include the stepwise use of analgesics (nonsteroidal anti-inflammatory drugs, opioids, and combinations thereof), as well as targeted hyperbaric oxygenation.
Recommended treatment modalities: As PG is an immunological disorder, specific therapy mainly involves substances that suppress or modulate the immune system. Corticosteroids, Antineutrophil agents, immunosuppressants and immunomodulators are recommended.
- Corticosteroids: Corticosteroids act through their anti-inflammatory and immunosuppressive properties, but one study suggests that corticosteroids may also restore monocyte function in this condition. Corticosteroids are prescribed in various ways, and all these methods can be used for all forms of PG.
- Antineutrophil agents have a beneficial effect based on the fact that the disease is primarily characterized by a neutrophilic dermal infiltrate. The main indication for these agents is their use to reduce steroid usage or in addition to steroids when the latter only provide a partial response. They are also used in non-aggressive disseminated disease and when local therapy is ineffective.
- Immunosuppressants and immunomodulators: The mechanism of action of these agents is related to the correction or modification of immunologic defects inherent in the disease. Immunosuppressants and immunomodulators are used as an adjunct or alternative therapy when systemic corticosteroids are ineffective or as first-line therapy with systemic steroids in aggressive disease.
Alternative and experimental treatment methods:
- Sodium cromoglycate: This drug is helpful when applied as a 1-4% solution three times a day as monotherapy for localized disease or as adjunctive therapy for disseminated disease.
- Thalidomide: The drug is prescribed at a dose of 150-400 mg per day. The main side effects are teratogenicity and neuropathy.
- Potassium iodide: Potassium iodide is prescribed at a dose of 300 mg 2 or 3 times a day. The main side effects are metallic taste in the mouth, arthralgia, and sometimes the possibility of neutrophilic dermatosis.
- Plasma exchange: Plasma exchange is performed three times a week, with a total of 4-27 procedures. The main side effects are disturbances in fluid and electrolyte balance, a tendency to bleeding, and infection.
- Intravenous immunoglobulin G: Intravenous immunoglobulin G is prescribed at a dose of 0.4 g/day for 5 days, followed by 0.1 g/day for 2 days after 2 weeks. The main side effects are high treatment cost, headache, and increased frequency of infections.
- 5-aminosalicylic acid: This drug is effective when locally applied daily to the affected areas as a 10% cream. Its mechanism of action is likely related to the suppression of leukocyte mobility and cytotoxicity.
- Nicotinic acid patch: Remission is observed with a dose of 6 g/day.
- Nitrogen mustard: Effective when applied as a 20% solution.
- Cytosine arabinoside and daunorubicin.
- Mycophenolate mofetil.