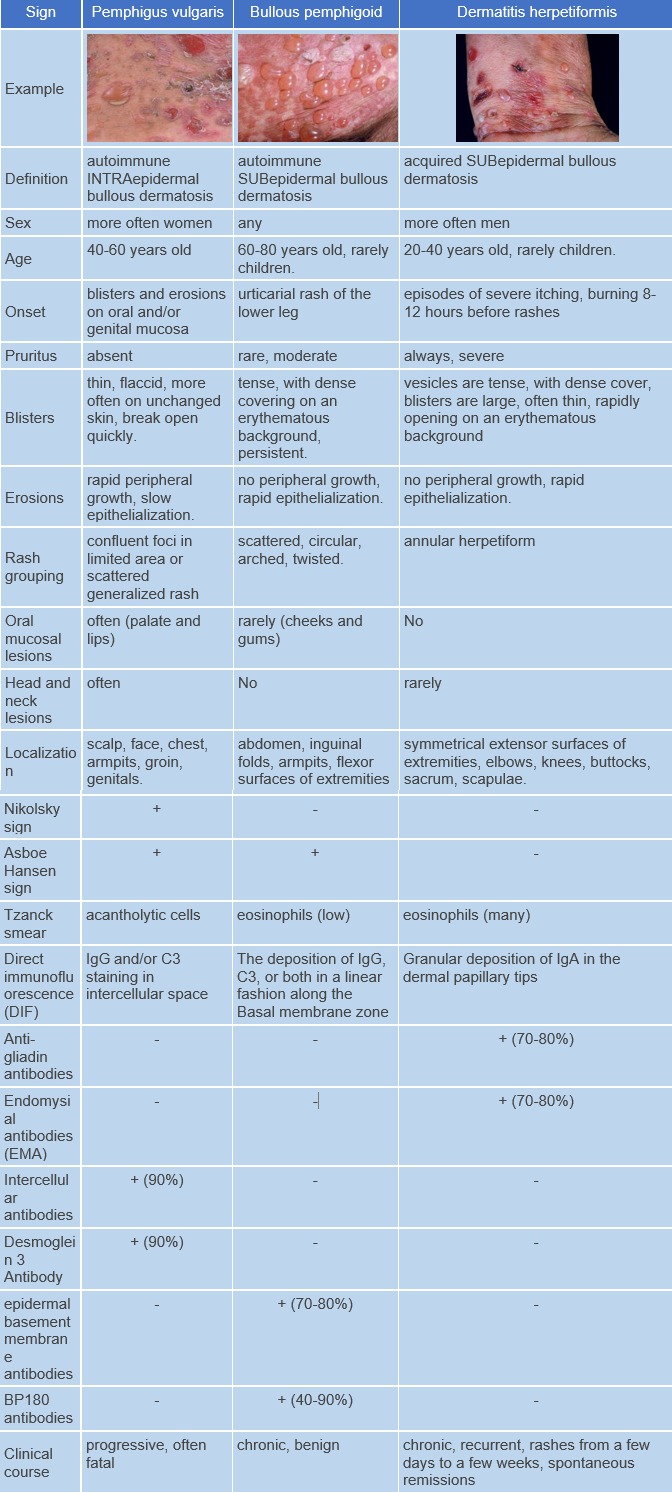
Dermatitis herpetiformis (dermatitis herpetiformis Duhring) is an inflammatory skin disease associated with gluten-sensitive enteropathy characterized by polymorphic pruritic eruptions, a chronic recurrent course, and granular deposition of IgA in the dermis. ICD-10 Code: L13.0
Dermatitis herpetiformis is a rare dermatosis that is more common in northern European populations. According to epidemiologic studies conducted in Northern Europe, the incidence varies from 0.4 to 3.5 cases per 100,000 population per year, and the prevalence ranges from 1.2 to 75.3 cases per 100,000 population. The disease typically begins in individuals between the ages of 30 and 40, but can also develop in children and the elderly. Males are more commonly affected than females, with the male-to-female ratio ranging from 1.1:1 to 1.9:1.
Dermatitis herpetiformis, like gluten-sensitive enteropathy (celiac disease), is associated with the HLA-DQ2 and HLA-DQ8 haplotypes. Approximately 5% of patients with gluten-sensitive enteropathy develop dermatitis herpetiformis. Possible mechanisms involved in the development of dermatitis herpetiformis in gluten-sensitive enteropathy include the following:
- After ingestion and digestion of gluten-containing food, gliadin is formed, which is absorbed through the mucosa of the small intestine.
- Gliadin is deaminated by tissue transglutaminase in the small intestinal mucosa, resulting in the formation of covalent cross-links between gliadin and transglutaminase.
- Deaminated gliadin peptides bind to HLA-DQ2 or HLA-DQ8 molecules on antigen-presenting cells, where they are recognized by Th-lymphocytes.
- Activated Th-lymphocytes produce pro-inflammatory cytokines and matrix metalloproteinases, which stimulate damage to the intestinal mucosa and the production of antibodies against tissue transglutaminase by B-cells.
- An immune response against an endogenous antigen or multiple endogenous antigens develops due to their exposure during tissue damage, leading to the production of IgA antibodies capable of binding to epidermal transglutaminase.
- IgA antibodies to epidermal transglutaminase circulate in the bloodstream, reach the skin, and bind to epidermal transglutaminase in dermal papillae.
- Deposition of immune complexes in dermis stimulates neutrophil chemotaxis, leading to proteolytic cleavage of the basement membrane at the lamina lucida level, resulting in the formation of subepidermal blisters.
The occasionally observed monomorphism of the eruptions allowed the identification of several clinical forms of the disease:
- Bullous form.
- Herpes-like form.
- Trichophytoid form.
- Strumous form.
The disease is characterized by a chronic relapsing course with alternating periods of medically induced or spontaneous complete remissions lasting from several weeks to several years. Spontaneous remissions are possible in 10-25% of patients. The disease is characterized by polymorphism, grouping and symmetry of the eruptions. The eruptions are predominantly localized on the extensor surfaces of the limbs, the hairy part of the head, shoulders, knees, elbows, sacrum and buttocks, accompanied by pruritus.
The rash consists of macules, vesicles, papules and blisters of various sizes. The blisters are tense, with a firm covering, filled with a clear or sometimes hemorrhagic content. They form on a hyperemic and edematous base. The blisters rupture, forming erosions that quickly epithelialize, leaving hyperpigmentation. Involvement of the oral mucosa is rare.The diagnosis is based on the analysis of anamnestic, clinical, and laboratory data.
For the diagnosis, the following laboratory tests are required:
- Examination of blisters for eosinophilia.
- Histological examination taken from a fresh lesion
- Direct immunofluorescence examination can reveal granular deposits of immunoglobulin class A in the dermis.
Serum blood tests using the indirect immunofluorescence method:
- Determination of IgA antibodies to tissue transglutaminase in the blood.
- Determination of IgA antibodies to endomysium in the blood.
To assess the patient's overall condition and detect associated conditions related to herpetiform dermatitis, additional investigations may be performed:
- Biopsy of the small intestine
- Assessment of malabsorption markers (iron levels, vitamin B12, folic acid in serum blood).
Screening for other autoimmune diseases:
- Determination of non-specific antibodies in the blood, such as antibodies to thyroperoxidase (detected in approximately 20% of patients with dermatitis herpetiformis) and antibodies to gastric parietal cells (found in 10-25% of patients with dermatitis herpetiformis), and antinuclear antibodies.
- Testing to detect thyroid diseases, including measuring levels of thyroid-stimulating hormone (TSH), total triiodothyronine (T3) in the blood, and total thyroxine (T4) in serum blood.
- HLA II typing for histocompatibility antigens: dQ2, dQ8.
Treatment goals:
- Stop the appearance of new eruptions.
- Epithelialization of erosions.
- Achieve and maintain remission.
- Improve the quality of life of patients.
General remarks on therapy:
- The basis of therapy is a gluten-free diet, which leads to the resolution of the cutaneous process, elimination of enteropathy, and disappearance of IgA antibodies to gliadin, endomysium, and tissue transglutaminase.
- The drug of choice for treating patients is dapsone. Dapsone therapy requires careful laboratory monitoring, especially of liver and kidney function. Serious side effects can occur, especially hemolysis. Severe hypersensitivity syndrome may also develop.
- In case of adverse effects during dapsone therapy or its ineffectiveness, sulfasalazine may be prescribed. On sulfasalazine therapy, hypersensitivity reactions, hemolytic anemia, proteinuria, and crystalluria may be observed. To monitor adverse effects of drug therapy, clinical blood tests and general urinalysis are prescribed before starting treatment and monthly for the first 3 months, then every 6 months. The most common adverse effects of sulfasalazine therapy - nausea, vomiting, and anorexia - can be avoided by prescribing enteric-coated formulations of the drug.
- Systemic glucocorticoid preparations are not very effective.
Diet:
The diet should completely exclude wheat, barley, rye, oats, and other grains. Products containing iodine (seafood, feijoa, persimmon, etc.) should also be excluded. A gluten-free diet results in resolution of flares within 1-2 years, but dermatitis herpetiformis invariably relapses within 12 weeks after reintroduction of gluten in the diet, so patients must adhere to the diet for life. Only 10-20% of patients develop immune tolerance and the ability to follow a regular diet after several years of strict gluten-free diet; this is most often observed in cases of childhood onset and in patients receiving dapsone. Long-term strict adherence to the gluten-free diet reduces the need for medication, reduces the risk of developing intestinal lymphoma, and resolves skin eruptions and symptoms of enteropathy/malabsorption.
Systemic Therapy:
- Dapsone: 1 mg per kg of body weight orally per day for 1-2 years (until a stable effect of a gluten-free diet is achieved).
- Sulfasalazine: orally in a dose of 1-2 grams per day.
Note: In the medical instructions for sulfasalazine, dermatitis herpetiformis is not listed as an indication for the use of the drug.
Antihistamines can be used to control itching, alternating as needed every 10 days:
- Clemastine: 1 mg orally twice a day for 7-10 days.
- Chloropyramine: 25 mg orally 1-2 times a day for 7-10 days.
- Loratadine: 10 mg once a day orally for 7-10 days.
- Mebhydroline: 50-200 mg orally 1-2 times a day for 7-10 days.
In case of severe itching, parenteral administration of antihistamines is indicated:
- Clemastine: 2 mg intramuscularly at night for 7 days, or
- Chloropyramine: 20-40 mg intramuscularly at night for 7 days.
Topical Therapy:
Topical glucocorticosteroid preparations can be used to reduce severe itching:
- Clobetasol propionate 0.05% ointment or cream on affected areas once a day, or
- Triamcinolone 0.1% ointment on affected areas twice a day, or
- Betamethasone 0.01% ointment on affected areas twice a day.
Treatment of Blisters and Erosions:
- Areas with blisters and erosions are treated with solutions of aniline dyes, and in the presence of secondary infection, aerosols containing glucocorticosteroids and antibacterial agents are used. Antiseptic solutions are used for rinsing erosions in the area of the oral mucosa.
Treatment for Children:
- The recommended dosage of dapsone for children is 2 mg per kg of body weight per day.
Approach in Case of Treatment Failure:
- In case of no response to dapsone therapy at a dosage of 1 mg per kg of body weight per day, the dosage of the drug can be increased to 150-200 mg per day for a short course, or sulfasalazine therapy may be prescribed orally.
Prevention:
- Primary prevention of dermatitis herpetiformis has not been developed. Secondary prevention involves patients with dermatitis herpetiformis and celiac disease adhering to a gluten-free diet.