Hyperhidrosis - excessive sweating due to hypersecretion of sweat glands. ICD-10 code: R61
Severe forms of hyperhidrosis affect 1% to 5% of the population, a significant proportion of whom are young. Pathological sweating often leads to the development of various dermatological conditions. Sometimes the intensity and character of sweating is so pronounced that it leads to the development of emotional and behavioral disorders and disrupts the social adaptation of affected individuals. Increased sweating can be either pathological or physiological.
Physiological hyperhidrosis is a protective response of the body to high ambient temperatures, physical exertion, emotional stress, consumption of large amounts of fluids, hot food, etc. Physiological sweating includes increased sweating in people during the initial stage of acclimatization, in overweight women during hyperthermia, during the premenstrual period, during menopause, and in the third trimester of pregnancy.
Pathological hyperhidrosis is caused by neuroendocrine disorders with predominant involvement of the central and autonomic nervous systems.
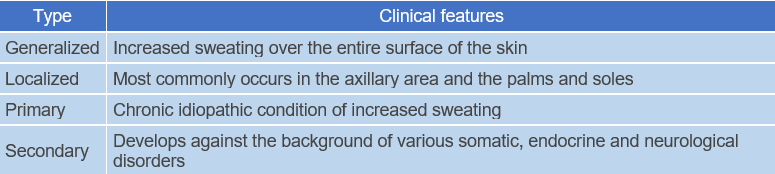
Classification:
- R61. Hyperhidrosis.
- R61.0. Localized hyperhidrosis.
- R61.1. Generalized hyperhidrosis.
- R61.9. Unspecified hyperhidrosis.
Disorders of sweating are frequently a part of the symptom complex of various nervous system and internal organ diseases.
Generalized hyperhidrosis is one of the symptoms of such diseases as diabetes, hyperthyroidism, obesity, as well as various infectious diseases. It is often observed in cardiovascular pathology, in weakened and debilitated individuals. The symptom of "night sweats" is well known in patients with pulmonary tuberculosis, chronic tonsillitis.
Localized (local) hyperhidrosis Increased sweating in a specific area of the body, often in the armpits, genital area, face, head, palms and soles. Localized hyperhidrosis is found in patients with hemiplegia, spinal cord lesions, syringomyelia, thrombophlebitis of the lower limbs.
Hyperhidrosis in the breast and groin folds leads to maceration and eczematization.
Hyperhidrosis of the hands is often associated with acrocyanosis and occurs mainly in young women. It is characterized by increased sensitivity of the hands to cold: the skin of the hands becomes covered with cold sweat with slight cooling, and the fingertips become red and shiny. Sweating changes the pH of the surface of the lipid mantle and creates conditions for viral, bacterial and fungal infections.
Hyperhidrosis of the feet can also be accompanied by acrocyanosis. Wearing non-porous footwear that impedes sweat evaporation worsens the condition, resulting in bacterial decomposition of sweat and a shift in the skin's acid-base balance toward alkalinity. This contributes to the softening of the stratum corneum and maceration. Lysis of bacteria and keratinocytes under the influence of sweat leads to the formation of an unpleasant odor. This process is particularly pronounced in individuals with flat feet.
Asymmetrical hyperhidrosis is observed in cases of organic lesions of the nervous system, such as spinal cord lesions and auriculotemporal syndrome.Minor's Test
The degree and area of hyperhidrosis can be approximated using the Minor's test (iodine starch test). In this test, Minor's reagent (2 grams of crystalline iodine, 15 ml of castor oil, and 90 ml of 96% ethanol) is applied to the area of skin to be examined. After the reagent dries, the area is dusted with starch. The result is assessed after 5-10 minutes.
When the reagent and starch come into contact with sweat, the area of skin takes on a color depending on the degree of sweating, ranging from blackish blue (heavy sweating) to pale blue (light sweating). The test can be used to determine the area of localized hyperhidrosis in the axillary region - spots up to 10 cm indicate mild hyperhidrosis, 10-20 cm indicate moderate hyperhidrosis, and over 20 cm indicate severe hyperhidrosis.Treatment of hyperhidrosis should be comprehensive and aimed at both the etiopathogenetic factor and the direct control of sweating.
Treatment of localized primary hyperhidrosis:
- Local antiperspirants and deodorants, which work by partially suppressing sweating through a coagulating effect or the deposition of insoluble compounds on the walls of sweat ducts and narrowing them.
- Aluminum chloride hexahydrate in a 20-25% solution of pure ethanol applied to the dry axillary area at night, with or without polyethylene occlusion, initially daily, and then every 2-4 weeks.
- Glutaraldehyde 10% for the palms and soles. Initially, the solution is applied every other day until control of the condition is achieved, then once a week or as needed.
- 10% methenamine.
- Locally astringent agents (solutions of boric, salicylic, acetic acids, tannin, alum, methenamine, formaldehyde, talc, etc.).
- Physiotherapeutic methods
- Iontophoresis is a simple and effective treatment for mild to moderate hyperhidrosis of the palms and soles. During the procedure, the patient's palms and soles are exposed to an electric current of 15-20 mA, which is delivered through a diluted solution of an anticholinergic drug or tap water (the mechanism of action of iontophoresis with tap water remains unknown). The duration of each procedure varies from 10 to 40 minutes, with an average session lasting 20 minutes. Usually, the condition normalizes with progressive treatment (2-6 sessions per week until achieving eugidrosis) and is maintained by repeating sessions every 3-6 weeks. The interval between two sessions should be constant, as there are no structural changes in the sweat glands. Theoretically, treatment should be continued indefinitely, although the condition usually improves with age.
- Electrophoresis of cholinolytics is recommended.
- Four-chamber baths and sea baths are effective.
- Medication treatment: anticholinergic drugs, sedatives, and β-blockers.
- Pachycarpine hydroiodide 0.1 g 2-3 times a day.
- Nanofin 0.1 g 2-3 times a day.
- Glycopyrrolate bromide in a dose of 2 mg 3 times a day.
- Good results are achieved with the administration of atropine, calcium chloride, and rutocide.
- For hyperhidrosis occurring in the context of emotional disorders, a pronounced effect is achieved with intravenous administration of tranquilizers (2-4 ml of 0.5% diazepam solution).
- Internally, taking sage and nettle infusion (15 g of dried leaves per 0.5 liters of water) in a dosage of 1/2 cup twice a day for 4 weeks is recommended; the treatment course can be repeated after 3-4 months.
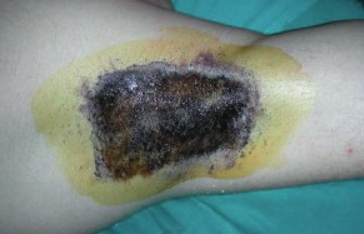
- Surgical treatment (excision of skin flaps or sympathectomy) is used only in severe cases of hyperhidrosis and provides a state of complete anhidrosis in the axillary and palmar areas. However, there is a risk of serious complications with surgical treatment, such as pneumothorax, bleeding, secondary infection, postoperative scarring, etc. Compensatory hyperhidrosis and dryness of the palms may also occur after surgery. Proper preventive and hygienic skin care is of great importance in the management of hyperhidrosis.
People who tend to sweat excessively should avoid wearing synthetic fabrics, especially in hot weather. Airbaths, baths, and contrast rubs are recommended. It is essential to take daily showers in the morning and evening with toilet soap, paying special attention to skin folds and changing clothes frequently. After washing, it is advisable to use special deodorants to eliminate body odor. It is also recommended to wipe the body with a weak solution of vinegar (1 part of white vinegar to 4 parts of water) or a decoction of 10% oak bark.
For excessive sweating of the hands, soaking them in a solution of saltpeter (1 teaspoon per 1 liter of water) can be helpful. People with sweaty hands and acrocyanosis should avoid work involving exposure to cold and moisture and wear gloves at low temperatures.
It is recommended to avoid activities that strain the hands, such as typing, electronics, precision mechanics, and jewelry making.
For sweaty feet, flat feet should be corrected and synthetic shoes, socks and stockings should be avoided. Feet should be washed daily with soap, dried thoroughly with a soft towel, and treated with antiperspirants. Because increased sweating can lead to maceration, erosion, and cracking of the skin, patients with hyperhidrosis should be examined by a dermatologist for early detection of fungal infections.
Botulinum toxin injection is a fundamentally new approach to treating localized hyperhidrosis. The mechanism of action of these preparations involves presynaptic blockade of acetylcholine release in cholinergic synapses. When the botulinum toxin type A-hemagglutinin complex (botulinum toxin, Dysport) is injected into the area of hyperhidrosis, it blocks the transport of acetylcholine, which is the mediator of sympathetic neurotransmission in sweat glands. As a result, sweating is reduced or completely stopped for a period of 6 to 12 months. This method provides achieving a long-lasting clinical effect without serious side effects or complications. Botulinum toxin injections should only be performed by trained medical professionals (dermatologists, neurologists) with experience and the appropriate authorization to use this method. The medical institution must have a license for medical activities.
When using this medical technology, the following contraindications are distinguished: Absolute contraindications: neuromuscular disorders, pregnancy, lactation, hemophilia, local inflammatory processes, increased sensitivity to the components of the preparation. Relative contraindications: the use of anticoagulants, exacerbation of somatic diseases, the use of antibiotics.
To perform the procedure, it is necessary to use Dysport containing 500 IU of botulinum toxin type A, which is diluted with 2.5 ml of 0.9% sodium chloride solution immediately before the procedure. The patient lies down during the procedure. Before administering the preparation, a preliminary test is recommended in the injection area to determine the area and intensity of sweating (Minor's test or hydrometry). After the treatment, sweating tests are repeated in dynamic. The choice of the optimal dose of the preparation depends on the area of injection and intensity of sweating. The effect of the preparation starts after 2-3 days and the maximum effect is observed after 2 weeks. The duration of the effect varies from 3 to 12 months - during this period complete anhidrosis or significant reduction of sweating is observed.