Glomus tumor, also known as glomus angioma, is a benign tumor arising from the arteriovenous anastomosis. ICD-10 code: D18.0
It can be observed at different ages without gender distinction and accounts for 1-2% of all soft tissue tumors. This organoid-type tumor develops from the walls of the Sucquet-Hoyer canal, which is a functional part of the glomus arteriovenous anastomosis. The tumor has a narrow lumen lined by endotheliocytes and surrounded by several layers of glomus cells, which are considered modified smooth muscle cells that alter the lumen of the anastomosis. Glomus bodies are highly innervated. Under normal conditions, glomus cells play a role in the regulation of body temperature and blood pressure. Glomus bodies are primarily concentrated in the acral areas (palms, soles, fingertips, and toes), which determines the predominant localization of tumors in these areas. However, they can also develop extra-acrally, possibly from myofibroblasts derived from neural crest stem cells during embryogenesis.
The etiology is not well understood. In most cases the tumors occur sporadically, but in a small proportion of cases they may be associated with trauma or pregnancy. Multiple lesions may be congenital or inherited as an autosomal dominant trait with incomplete penetrance and variable expressivity.
Classification: There are two forms of glomus tumor:
- Isolated (solitary)
- Multiple disseminated
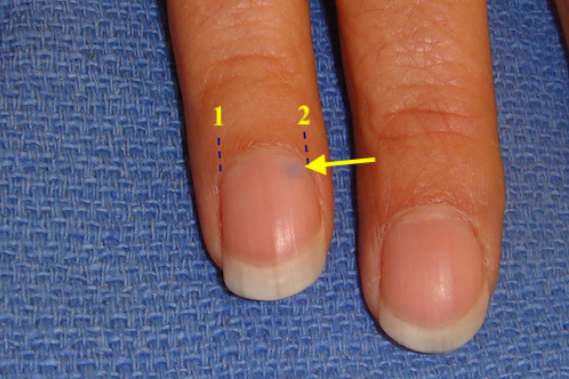
Isolated (solitary) form: Solitary glomus tumors are the most common (90% of all cases) and are predominantly located on the acral areas, especially subungually on the fingertips. Subungual tumors appear as pink to purple nodules 3-10 mm in diameter, rarely larger. They can be seen through the nail plate, causing thinning and longitudinal or transverse grooves. These tumors are more common in women between the ages of 20 and 40. In other acral and extra-acral areas (often on the limbs), the neoplasms are larger (up to 2 cm or more), mobile, well-defined, and dome-shaped. The nodules are firm, pink to reddish-purple in color, and may be painful to palpation. They are located in the skin or subcutaneous tissue and sometimes have a mushroom-like shape.
Extra-acral glomus tumors are located on the shins, thighs, trunk, and in some cases have unusual localization, such as
- Oral cavity
- Periurethral region in women, accompanied by ulceration and vaginal bleeding
- Glans penis or corpora cavernosa, often leading to priapism
- Lumbar-sacral area, causing coccydynia
The classic triad of symptoms includes painful palpation of the tumor, increased sensitivity to cold, and intense spontaneous pain episodes that occur paroxysmally and last up to 1 minute. However, these episodes may recur several times within a day, causing anxiety and emotional instability in affected individuals.
Multiple disseminated form: Multiple glomus tumors account for about 10% of cases. Unlike solitary tumors, they can be familial, autosomal dominant, congenital, and very rarely acquired. If they appear in childhood, they become more pronounced in adolescence.
The distribution of multiple glomus tumors may be localized, segmental, or disseminated. The most commonly affected areas are the trunk and upper extremities, but the face, scalp, genital organs, and occasionally the oral mucosa (gums, inner surface of the lips) and muscles may also be involved.
Two forms are distinguished: nodular and plaque-like.
In the nodular form, the clinical manifestations are similar to those of solitary glomus tumors. The tumors are softer, with a pink, dark blue, or purple color, sometimes with a hyperkeratotic surface. Starting as single nodules, they gradually become multifocal and their number can range from a few dozen to hundreds over time. In some patients, dissemination occurs throughout life.
The plaque-like form is rarer and predominantly congenital. It is characterized by flat, larger tumors that gradually change color to darker shades.
Both forms are characterized by little or no pain on palpation. Pain is present in only 40-60% of patients. Visceral involvement is also possible.- Neuromas
- Angioleiomyoma
- Foreign body granuloma
- Blue rubber bleb nevus syndrome
- Blue nevus
- Hemangiomas
- Angiolipoma
- Hemangiopericytoma
- Epidermal cyst
- Metastases
- Sarcoidosis
- Eccrine spiradenoma
- Melanoma
Treatment of solitary forms typically involves surgical excision, although recurrences occur in 12-33% of cases and some patients may develop multiple tumors. Laser therapy (CO2, Argon, Nd:YAG laser) is used to remove small, superficial neoplasms.
For multiple tumors, sclerotherapy (injection of sodium tetradecyl sulfate, polidocanol, hypertonic solution) or staged surgical excision is used.