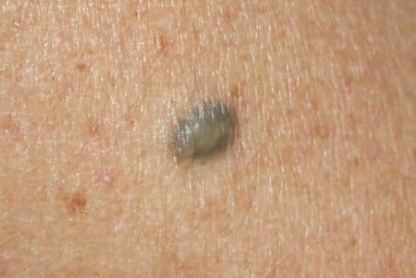
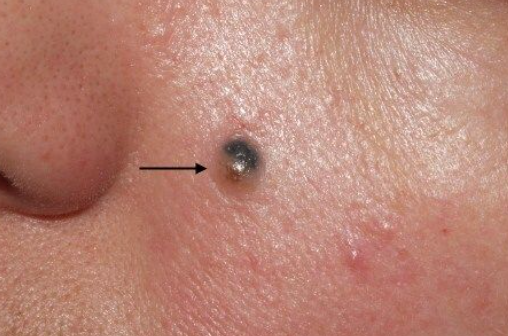
Common Blue Nevus
Characterized by small (0.5-1.0 cm in diameter), well-demarcated, dome-shaped, firm papules or nodules with a smooth, hairless surface, ranging in color from blue, bluish, dark blue, gray to blue-black. A characteristic feature of the nevus is the preservation of the skin pattern on its surface. Localization can be anywhere, but in half of the cases the nevus is found on the dorsal surfaces of the feet and hands. Less often it appears on the buttocks, trunk, scalp and face. The growth is slow and there is no malignant transformation. With age, it may flatten and become lighter, but complete regression of the tumor is not observed.
Hypomelanotic (Amelanotic) Blue Nevus
Occurs between the ages of 20-40, and is more common in women than in men. It is characterized by a small (up to 1 cm in diameter), asymptomatic, firm, dome-shaped papule with a smooth surface and a flesh-colored appearance. In some cases, hyperpigmented spots may be observed on the surface of the papule. It is often located on the scalp and the distal parts of the extremities. This is considered a rare variant of blue nevus, but its prevalence is likely underestimated due to its lack of symptoms and misdiagnosis. The diagnosis is typically established through histological examination.
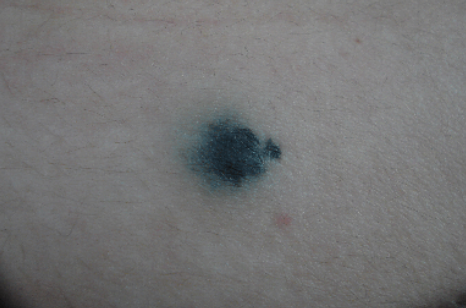
Plaque-like Blue Nevus
Characterized by irregularly shaped spots or flat plaques with a smooth surface, ranging in size from a few millimeters to 10 centimeters, with varying shades of blue. The spots are not palpable and the plaques have a moderately firm consistency. It can be found anywhere on the body, but is more common on the buttocks, extremities, and face.
Targetoid Blue Nevus
An unusual variant of the blue nevus in the form of a hyperpigmented dome-shaped formation, located at the center of a lighter-colored spot or plaque.
Oral Blue Nevus
Usually presented as spots or flat plaques of round or irregular shape, with blue or bluish colors of various shades on the hard palate, inner surface of the cheeks, sclera, penis, vulva and cervix. It is detected in mature age and may appear suddenly. These patients have an increased risk of developing melanoma.
Grouped Blue Nevus
Multiple blue nevi presented as spots or flat plaques with varying degrees of hyperpigmentation, grouped in clusters, but isolated from each other. It may resemble nevus spilus or coexist with them. Commonly located on the scalp.
Eruptive Blue Nevus
Characterized by the eruption of multiple typical blue nevi within one anatomical area, either segmentally or generalized. Familial blue nevi inherited in an autosomal dominant manner and present from birth, as well as sporadic cases, have been reported.
LAMB Syndrome
Also known as the complex Carney or NAME syndrome. It consists of lentigos, cardiac and/or mucocutaneous myxomas, mucoid neurofibromas, freckles, and blue nevi, which are usually solitary or more commonly multiple simple or speckled forms with a frequency of 40-50%.
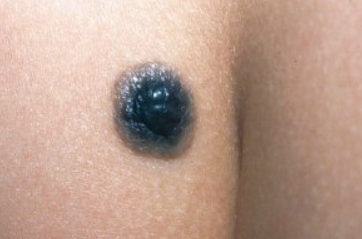
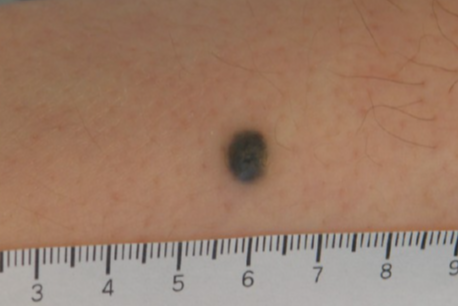
Cellular Blue Nevus
Cellular blue nevus is a variant of blue nevus characterized by an abundance of cellular elements. Clinically, it is often considered a malignant lesion due to its large size (ranging from 5 mm to 3 cm in diameter) and marked pigmentation. Typically, the lesion appears as a blue nodule with a smooth or uneven surface. In half of the cases it is localized on the skin of the buttocks and lumbosacral area, less frequently on the dorsal surfaces of the feet, hands, scalp and face. It can be congenital, appearing in childhood and adulthood, and is more common in women.
Atypical Cellular Blue Nevus
It occupies an intermediate position between the typical form of cellular blue nevus and its malignant form or melanoma arising from a blue cellular nevus. Atypical features include advanced age, rapid tumor growth (more than 5-10 cm), ulceration, color change, and histologically, pronounced nuclear pleomorphism and a mitotic rate of 3-4 per square millimeter.
Giant Cellular Blue Nevus
In some cases, the nevus can reach large sizes, up to 10 cm or more in diameter, but its slow growth does not indicate malignant transformation.
Masson Nevus (Blue Cellular Neurocristic Hamartoma)
A rare variant of cellular blue nevus with Schwannian differentiation, clinically characterized by a deep-seated, bluish-gray nodule, usually located on the buttocks. The diagnosis is established histologically.
Amelanotic (Hypomelanotic) Cellular Blue Nevus
A blue nevus without melanin synthesis. The clinical presentation is similar to a simple non-pigmented blue nevus, but the cellular nevus is larger, measuring 1 cm or more, and tends to ulcerate. Immunohistochemical examination shows a positive reaction for S-100 protein and HMB-45.
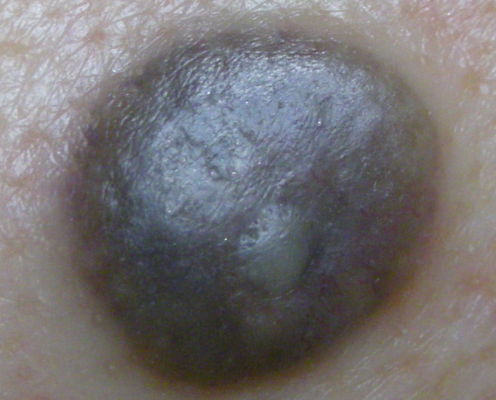
Sclerosing Cellular Blue Nevus
Sclerosing blue nevus, also known as desmoplastic blue nevus, clinically presents as a single, dome-shaped, firm papule or nodule, measuring 1-3 cm. A characteristic feature is the amorphous blue color with various shades in the peripheral part of the lesion, while the center is hypopigmented, which is well observed on dermatoscopy.
Combined Blue Nevus
Blue nevi are a common component of combined nevi. They are observed in combination with borderline, intradermal, and complex melanocytic nevi and very rarely with Spitz nevi. Clinically, this diagnosis is challenging, and histological examination is required. An exception is the combination with nevus spilus when melanocytic and blue nevi are simultaneously observed in the area of a "café u latte colored patch.
Epithelioid Blue Nevus (Pigmented Epithelioid Melanocytoma)
Also known as "animal-type melanoma" (observed in horses and rodents) and "epithelioid blue nevus of the Carney complex" (first detected in this condition). To date, it has been described in patients without an association with the complex and with frequent metastases to lymph nodes. Clinically, it appears as a slowly growing or recently changed pigmented macule or dermal nodule with a blue or blue-gray color. It is mostly found in children, adolescents, and young adults. In most cases, the neoplasm arises de novo (on unaffected skin), but it can sometimes occur in the area of melanocytic nevi.
Deep Penetrating Nevus
Also known as plexiform spindle cell nevus, it is a combination of structures from several melanocytic nevi: blue, complex, and Spitz nevi. It usually develops between the ages of 18 and 30, and in only 5% of cases it occurs in individuals older than 50, more commonly in women. Clinically, it presents as an asymptomatic single flat pigmented macule or dome-shaped papule up to 1 cm in size, ranging in color from blue to black, depending on the predominant component. Cases with a pink hue have also been described. Common sites include the face, neck, shoulder girdle, and less commonly the upper and lower extremities, scapular area, and abdomen. A characteristic feature of this nevus is its sudden appearance and rapid growth.
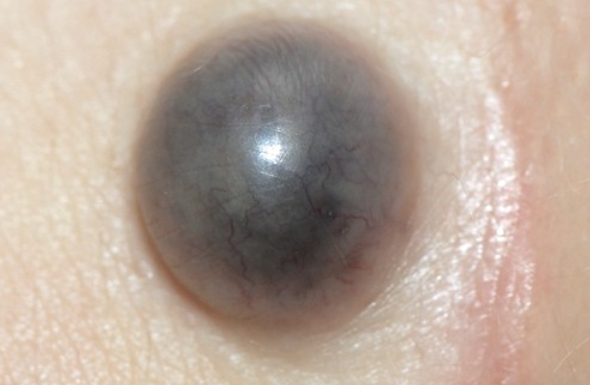
Malignant Blue Nevus
Also known as "blue" melanoma. It occurs between the ages of 22 and 73, with 65-70% of cases in males. It most often develops on the background of a long-standing cellular blue nevus that has been present for several years. In rarer cases, it arises de novo (on unaffected skin) and immediately exhibits pathomorphological features resembling a cellular blue nevus. It typically presents as a flat macule with varying degrees of pigmentation, ranging from blue to blue-black, and an irregular shape, measuring over 2 cm. The surface is non-uniform, often with blue-black papules, nodules, and ulcerations. Common sites include the face, scalp, upper chest, and less commonly the extremities. Distant metastases to the liver, lungs, lymph nodes, brain, and bones are observed in the first two years. The tumor size is usually more than 2 cm in diameter, and ulceration is seen in 26% of cases. The prognosis is poor and the average life expectancy rarely exceeds 3 years.