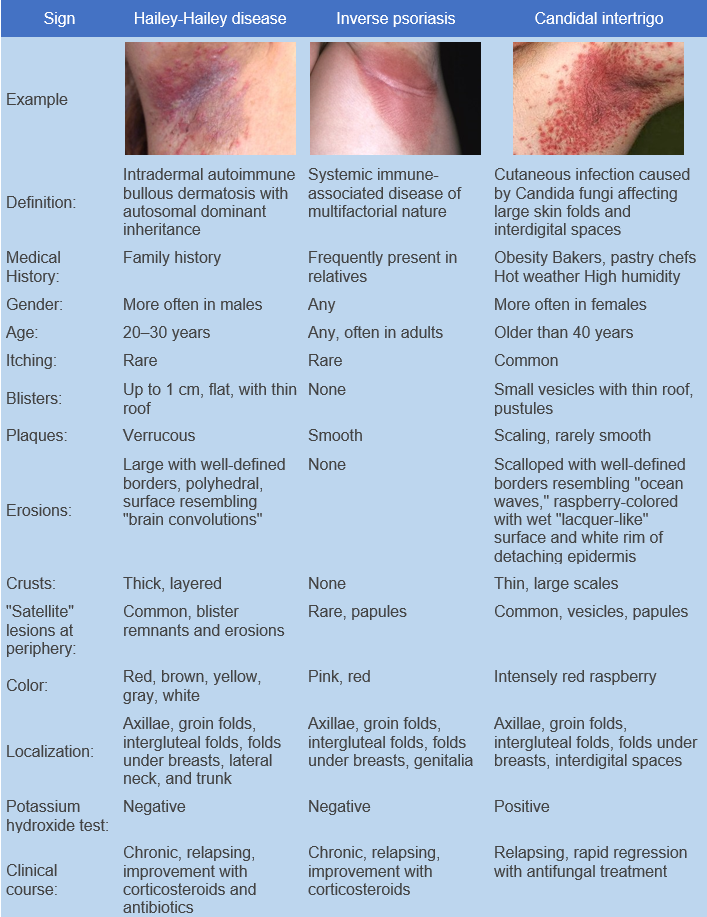
Candidal intertrigo is a skin infection caused by Candida fungi, affecting large skin folds and interdigital spaces. ICD-10 code: B37.2
Individuals predisposed to infection include older women with sagging breasts, overweight men, and women with hanging skin folds in the lower abdomen, groin, rectal, and axillary areas. Predisposing factors include hot weather, high humidity, tight or abrasive clothing, diabetes, and poor hygiene.<.p>
Inflammatory conditions in the skin folds, such as psoriasis, and the use of topical steroids promote fungal growth in the folds. Obese diabetics are prone to recurrent candidal infections. Involvement of the interdigital folds of the hands is uncommon but typically occurs in adults, usually women who are housewives or work in the food processing or bakery industries.<.p> Yeast-like fungi tend to thrive in intertriginous areas that retain heat and moisture, creating an environment conducive to fungal infections.
The condition is characterized by the appearance of small blisters with a thin, easily ruptured roof on an erythematous base in the axillary, groin, intergluteal, and submammary folds. These blisters evolve into erosions that rapidly increase in size, forming extensive eroded raspberry-colored areas with a moist shiny ("lacquer-like") surface that may completely occupy the contacting fold surfaces.
A narrow band of detached epidermis is visible at the edge of the erosive areas. The border of the lesion is long, well defined, with macerated scales along the edge, resembling a wavy ocean coastline. Erosive areas may alternate with areas of macerated epidermis, which are characterized by a whitish color and marked thickening. There is a tendency to develop painful fissures. Erosion and maceration of the epidermis are confined to the contacting surfaces of the folds.
Healthy skin adjacent to the main affected areas almost always shows scattered small vesicles, papules, pustules, or erythematous and scaly eruptions.
In cases of interdigital involvement, only one fold is usually affected, more commonly on the right hand between the middle and ring fingers. Pustules develop and rupture to form erosions or fissures. The affected area is surrounded by a white rim of thickened epidermis and is often associated with candidal paronychia.
The condition may persist and recur after treatment.The diagnosis is based on clinical data and microscopic and/or cultural examination.
KOH examination is performed by obtaining material from pustules or the advancing border of the lesion using a cotton swab or a gentle scrape with a No. 15 surgical scalpel blade. The material is placed on a microscope slide, 10% potassium hydroxide solution is added, and a cover slip is placed over it. The material is gently pressed to distribute it for better examination. Slightly heating the sample is optional but often unnecessary. There are often numerous pseudohyphae and spores.- Inverse psoriasis (can be associated with superficial candidal superinfection, especially after topical steroid treatment).
- Seborrheic dermatitis (typically affects the scalp, face, and fold areas).
- Contact Dermatitis in fold areas due to other causes (especially if potassium hydroxide examination is negative).
- Erythrasma caused by Corynebacterium (coral-red fluorescence under Wood's lamp).
- Eczema can mask superficial Candidal infection.
- Bacterial Intertrigo.
- Hailey-Hailey disease.
- Scabies (when involving interdigital folds).
Antifungal creams containing terbinafine ("Terbinafine"), miconazole, clotrimazole, ketoconazole, oxiconazole, econazole. Apply thinly twice a day for creams and once a day until clear for ointments.
In resistant cases, fluconazole ("Fluconazole") may be prescribed at a dose of 100 mg per day for 7 days. There is a potential interaction between systemic hypoglycemic agents and fluconazole, requiring careful blood glucose monitoring when used concomitantly.
An absorbable powder, not necessarily containing an active ingredient, may be used after the inflammation has resolved. The powder absorbs a small amount of moisture and acts as a dry lubricant, allowing skin surfaces to glide freely and preventing moisture accumulation in potentially stagnant areas.