Lupus erythematosus is a multifactorial autoimmune inflammatory connective tissue disease that affects various organs and systems and presents with a wide spectrum of clinical manifestations. ICD-10 Code: L93.
The etiology of discoid lupus erythematosus is unknown. Key elements in the pathogenesis of the disease include the impact of ultraviolet radiation, the formation of autoantibodies, the development of autoimmune reactions, disruption of T-lymphocyte and dendritic cell functions regulation. Risk factors for its development include prolonged exposure to sunlight, cold, wind (agricultural workers, fishermen, construction workers), skin phototype I, drug intolerance, and the presence of chronic infection foci.
Factors that trigger the development of cutaneous forms of lupus erythematosus include ultraviolet radiation, certain medications (terbinafine, tumor necrosis factor-alpha inhibitors, anticonvulsants, proton pump inhibitors, calcium channel blockers, angiotensin-converting enzyme inhibitors, beta blockers, leflunomide, etc.), viral infections, and skin injuries. Approximately 1/3 of subacute cutaneous red lupus cases are drug induced. Smoking is associated with an increased risk of developing cutaneous forms of the disease and a more severe course of the disease. Changes in the levels of sex hormones (estrogens) also play a significant role in predisposing to the disease.
The incidence of cutaneous forms of lupus erythematosus is 3.0-4.2 cases per 100,000 population per year, with the discoid form accounting for 70-80%. Onset is most common between the ages of 20 and 40, and women are more often affected than men.
Classification:
- Acute cutaneous lupus erythematosus:
- Localized
- Generalized
- Toxic epidermal necrolysis-like
- Subacute cutaneous lupus erythematosus:
- Annular
- Papulosquamous/psoriasiform
- Bullous
- Toxic epidermal necrolysis-like
- Chronic cutaneous lupus erythematosus:
- Discoid:
- Localized
- Generalized
- Hypertrophic/verrucous
- Deep/lupus panniculitis
- Tumidus
- Chilblain lupus
- Oral Lupus Erythemathosus (oral cavity, nose, genitals, conjunctiva)
- Cutaneous lupus erythematosus/lichen planus overlap syndrome
- Discoid:
Cross-manifestations of skin lesions are frequently observed in patients with cutaneous forms of lupus erythematosus (LE). Two or more clinical forms of cutaneous LE are observed in 35% of patients, acute cutaneous LE associated with discoid cutaneous LE in 30%, with subacute cutaneous LE in 14%, and with both discoid and subacute cutaneous LE in 15% of patients.
The likelihood of developing systemic lupus erythematosus (SLE) is up to 90% with acute cutaneous LE, 35-50% with subacute cutaneous LE, approximately 20% with widespread forms of chronic cutaneous LE, and no more than 5% with localized discoid cutaneous LE.
Discoid lupus erythematosus
Characterized by a triad of symptoms: erythema, hyperkeratosis, and atrophy. Lesions may be localized (mainly on the face, including the cheeks, nasal wings and ears, and the hairy part of the scalp) or widespread. Reddish patches appear on the skin that slowly increase in size, become infiltrated, and transforming into elevated plaques. In the central part of these plaques, follicular hyperkeratosis develops initially and then becomes continuous. The scales are difficult to remove and are painful to scrape. On the underside of the removed scale, keratin spicules are found embedded in enlarged follicular openings. A zone of active inflammation remains at the periphery of the lesions, accompanied by hyperpigmentation. The plaques gradually enlarge, and in the central area there is a disintegration of the elements, forming a coarse, indented, disfiguring scarred atrophy of the skin, which may be accompanied by telangiectasias.
In the vermilion border of the lips, eruptions are represented by slightly infiltrated cherry-red spots, covered with a small amount of scales that are difficult to remove.
Deep Lupus Erythematosus (Lupus Panniculitis)
Hypertrophic lupus erythematosus (verrucous lupus erythematosus)
Chilblain lupus
Lupus tumidus
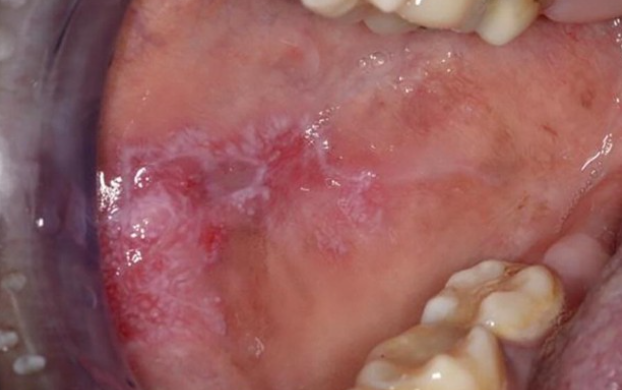
Oral lupus erythematosus
Psoriasiform lupus erythematosus
Annular Lupus Erythematosus
Bullous lupus erythematosus
Poikilodermatous Lupus Erythematosus
Erythrodermic Lupus Erythematosus
Pigmented (Melanotic) lupus erythematosus
Comedonal lupus erythematosus
Rowell syndrome
Lupus mastitis
Overlap syndrome lupus erythematosus/lichen planus
Represents a true combination of lupus erythematosus and lichen planus in which patients have symptoms of both diseases simultaneously. Clinically, eruptions are characterized by large atrophic hypopigmented patches or patches of red or pink color. Over time, the hypopigmentation of the affected areas intensifies with the appearance of desquamation and telangiectasias. Cutaneous eruptions are usually localized on the mid-back and extensor surfaces of the limbs.
A prominent palmoplantar keratosis is characteristic. Atrophy or complete absence of nails is common. Some patients may have scarring alopecia and areas of oral mucosal involvement.Acute cutaneous lupus erythematosus
Always represents a manifestation of systemic lupus erythematosus that manifests with skin involvement in 70-85% of cases. It is characterized by the development of erythema with a cyanotic center and swelling on the skin of the face in the area of the cheeks, cheekbones, and nose ("butterfly rash"). Less commonly, widespread maculopapular eruptions are observed. The rash elements usually appear after sun exposure, last a few days, and resolve, leaving minor hyperpigmented spots.
A unique equivalent of the "butterfly" is centrofacial erythema, which appears in the cheek area as slightly edematous, bright erythematous spots that slowly increase in size due to peripheral growth and simultaneously resolve in the central part. The red border of the lips may be involved, facial swelling may occur, and widespread maculopapular eruptions may occur on symmetrical areas of the skin.
Involvement of the mucous membranes of the oral cavity, hard palate, and nose may result in erosions and ulcerations. Rarely, the clinical picture of acute cutaneous lupus erythematosus may resemble toxic epidermal necrolysis.Neonatal Lupus Erythematosus
Scarring alopecia
Nail involvement in lupus erythematosus
The diagnosis of lupus erythematosus is based on the characteristic clinical picture, histological changes, and results of immunological tests.
Blood tests for all cutaneous forms of lupus erythematosus should include:
- Complete blood count (CBC) and urinalysis.
- Determination of blood biochemical markers: ALT, AST, γ-glutamyl transpeptidase, alkaline phosphatase, urea, creatinine, C-reactive protein.
- Immunological tests: antinuclear antibodies (ANA) - if positive, further testing includes antibodies to extractable nuclear antigens (ENA) and double-stranded DNA (anti-dsDNA), antibodies to nucleoproteins - anti-Ro/SS-A and anti-La/SS-B, antiphospholipid antibodies (via enzyme-linked immunosorbent assay), and precipitation reaction with cardiolipin antigen - VDRL.
- In cutaneous forms, autoantibodies may be produced. Patients with the discoid form exhibit the formation of anti-Ro/SS-A, anti-La/SS-B, and anti-annexin-1 antibodies. The majority of patients with subacute cutaneous lupus erythematosus show anti-Ro/SS-A (70%), ANA (60-80%), and anti-La/SS-B (30-50%) antibodies. When performing differential diagnosis, it is essential to consider that systemic lupus erythematosus is characterized by the presence of antibodies to the extractable nuclear antigen Sm (Smith) - anti-Sm and positive tests for anti-dsDNA.
- Polymorphic photodermatosis
- Lymphocytoma cutis (pseudo-lymphoma)
- Pemphigus erythematosus
- Erythema annulare centrifugum
- Rosacea
- Perioral dermatitis
- Seborrheic dermatitis
- Dermatomycoses (ringworm, tinea, favus)
- Granuloma faciale
- Sarcoidosis
- Psoriasis
- Lupus vulgaris
- Pseudopelade of Brocq
- Jessner's lymphocytic infiltrate
- Erysipelas
Treatment Goals:
- The goal is to achieve disease remission.
General Remarks on Therapy
Patients are treated with systemic antimalarials and topical glucocorticosteroids.
In cases of localized skin involvement, topical glucocorticosteroid preparations are prescribed. Creams and ointments are used for lesions on the body skin, and lotions are used for lesions on the scalp.
Antimalarial agents are effective both in combination therapy and monotherapy. Hydroxychloroquine sulfate is preferred due to better tolerability. Ophthalmologic examination is performed before starting antimalarial treatment and at least once every 6 months to monitor the possible development of retinopathy. Regular monitoring of laboratory parameters is also performed. In cases of resistance to antimalarial drugs, back-up drugs such as dapsone, retinoids or methotrexate are used. Systemic retinoids are indicated for severe hyperkeratosis (discoid, verrucous). The bullous form is treated with dapsone, which suppresses neutrophil migration, and systemic glucocorticosteroids.
Indications for Hospitalization
- Severe course of dermatosis.
- Lack of effect from outpatient treatment.
Treatment Regimens
Topical Glucocorticosteroids
For skin lesions localized on the face, it is recommended to use low or moderate potency topical glucocorticosteroids:
- Fluocinolone acetonide, cream, gel, ointment, lotion, applied to the lesions twice a day for 12 weeks.
Moderate potency topical glucocorticosteroids are recommended for lesions on the trunk and extremities:
- Triamcinolone, ointment, applied twice a day under occlusion to the lesions for 1 week, or.
- Betamethasone, cream, ointment, applied twice a day to the lesions for 8 weeks
For eruptions located on the scalp, palms, and soles, high potency topical glucocorticosteroid are recommended:
- Clobetasol propionate, cream, ointment, applied twice a day to the lesions for 4 weeks.
Intralesional injection of glucocorticosteroids may be used for localized refractory lesions. The use of this method is limited due to the risk of persistent atrophy.
- Triamcinolone Acetonide, 5-10 mg per mL, intralesional injection, or
- Betamethasone, 0.2 mL per cm2, intralesional injection, with a weekly dose not exceeding 1 mL.
An interval of no less than 4 weeks between injections is recommended if the need for intralesional injections persists.
Systemic Therapy
Antimalarial Drugs:
- Hydroxychloroquine, 5-6 mg per kg per day orally (or 2 tablets of 200 mg each for an adult of average weight). After achieving a clinical response, the dosage of hydroxychloroquine may be gradually reduced to 200 mg per day, continuing therapy for at least 2-3 months. Treatment with the drug may continue for 2-3 years. A 2.5-fold increase in the risk of recurrence occurs when discontinuing maintenance doses.
- Alternatively, chloroquine, 250-500 mg orally daily for at least 2-3 months. Treatment with the drug may continue for 2-3 years.
Considering the important role of ultraviolet-induced free radical damage to membranes and microcirculation disturbances in the pathogenesis, the inclusion of antioxidants in the treatment regimen is recommended: (Low evidence. Need more investigations)
- Vitamin E, 50-100 mg per day orally in intermittent courses: 1 week of drug intake, followed by 1 week of break, for 4-8 weeks.
Angioprotectors and microcirculation correctors are also recommended: (Low evidence. Need more investigations)
- Pentoxifylline, 200 mg orally 3 times a day for 1 month.
- Nicotinic acid, 0.05-0.1 g orally 2-3 times a day for 21-30 days, or 2-3 ml intramuscularly every other day, with a course of 8-10 injections.
Special Situations
Treatment for pregnant women is limited to topical corticosteroids of class I or II. The use of antimalarial drugs is contraindicated due to the possibility of fetal anomalies.
Approach in the Absence of Treatment Efficacy
Second-line drugs prescribed in the absence of effectiveness of topical glucocorticosteroids are topical calcineurin inhibitors:
- Tacrolimus, 0.1% ointment applied twice a day to the lesions for 4-8 weeks.
- Pimecrolimus, 1% cream applied twice a day to the lesions for 4-8 weeks.
Second-line systemic therapy includes retinoids. Treatment should start with lower doses (10-20 mg per day) and gradually increase based on tolerance and absence of side effects:
- Acitretin, 50 mg per day orally for 8 weeks, or
- Acitretin, 0.2-1.0 mg per kg body weight per day orally for 8 weeks, or
- Isotretinoin, 0.2-1.0 mg per kg body weight per day orally for 8 weeks.
Prevention
All patients are advised to take measures to protect their skin from the sun: wearing hats, clothing with long sleeves, closed necklines, pants and long skirts, regular application of sunscreen creams with a high SPF index (>50).