Lichen planus is a chronic inflammatory condition of the skin and mucous membranes, less commonly affecting nails and hair, characterized by typical papules. ICD-10 code: L43.
It is most common in people between the ages of 30 and 60. Women account for 60-75% of patients with oral mucosal involvement and about 50% of those with cutaneous involvement. Red flat lichen is rare in children, accounting for only 5% of cases in pediatric patients.
The etiology of the disease is unknown. It is thought to be an autoimmune disease in which expression of an unidentified antigen by basal layer keratinocytes leads to activation and migration of T lymphocytes into the skin, triggering an immune response and inflammatory reaction. Antibodies to hepatitis C virus have been detected in 16% of patients with cutaneous lichen planus and approximately 30% of patients with mucosal involvement. A positive family history is present in 10% of patients.
Often, a mnemonic (5 P) is used to describe the skin lesions associated with LP
- P - Pruritic (itchy)
- P - Planar (flat surface of eruptions)
- P - Polygonal
- P - Purplish-violet
- P - Papular
The course of lichen planus with skin involvement is usually favorable. Spontaneous remissions of skin lesions within 1 year after manifestation are observed in 64-68% of patients.
Papular (classic) lichen planus
Skin lesions in the typical form of lichen planus are characterized by monomorphic flat papules, 2-5 mm in diameter, polygonal in shape, with central depression, pink-red color with a characteristic purple or lilac tint, and a waxy sheen that is more pronounced on lateral illumination. Scaling is usually minimal. A reticular pattern (Wickham's striae) may be seen on the surface of larger papules, especially after wetting with water or petroleum jelly.
A characteristic feature of lichen planus is its tendency to form grouped eruptions, forming rings, garlands, or lines. Less commonly, papules coalesce to form plaques with a pebbly surface. New papules may appear around these plaques, densely or sparsely distributed. In most cases, the rash is symmetrical and often occurs on the inner surface of the forearms, wrists, sacrum, shins, and (especially in men) the genitalia. In some cases, rashes may spread over the entire skin, often to the oral mucosa. The palms, soles, and face are rarely involved. During exacerbations, Koebner's phenomenon may occur, where new nodules develop at sites of skin trauma. Patients may experience pruritus. In some cases, the disease occurs without itching.
Lichen planus usually resolves with the formation of secondary hyperpigmented patches, and sometimes hypopigmentation may remain.
Hypertrophic lichen planus
Characterized by formation of plaques with rounded or oval outlines measuring 4-7 cm or more in diameter. Color of these plaques is livid with a purplish tinge. The surface of the plaques is uneven, warty, covered with verrucous projections and numerous depressions. Small purplish-red nodules, characteristic of typical form, may be found at the periphery of main lesions. The lesions are usually localized on the anterior surface of shins, are intensely pruritic, and respond poorly to treatment.
Isolated hyperkeratotic lesions are sometimes seen which, when located on face and upper extremities, clinically resemble senile keratosis or basal cell carcinoma.Atrophic lichen planus
Lichen planus pigmentosus
Characterized by multiple brownish macules that coalesce into diffuse, occasionally limited reticular, patchy, unilateral linear, and perifollicular lesions. There are typical papules as well as pigmented elements. Common sites include face, neck, and upper extremities, and less commonly, skin folds and creases.
These patches and papules are ash-black, dark brown, brownish-blue in color, irregular in shape and size, and in the early stages have a narrow reddish border. The eruptions are often asymptomatic, sometimes accompanied by pruritus. Lesions progress slowly with no tendency for spontaneous resolution.
Histologically, there is epidermal atrophy, vacuolation of the basal layer, and moderate lymphohistiocytic infiltration in the dermis.Bullous lichen planus
Clinically characterized by formation of vesicles or bullae on plaques and papules on erythematous areas or unaffected skin. The eruptions vary in size and have a thick tense covering that later becomes flaccid and wrinkled. The contents of the vesicles are transparent, slightly opalescent with a yellowish hue, and in some places, contain blood. A distinctive feature of the condition is appearance of blisters both within area of lichen planus plaques and on healthy skin.
Blisters can also appear on oral mucosa, sometimes in isolation, which can complicate the differential diagnosis with pemphigoid. Blisters forming on normal skin are a more characteristic symptom of the pemphigoid variant, and they should be differentiated from the bullous form using direct and indirect immunofluorescence tests.Erosive-ulcerative lichen planus
Characterized by development of erosions on the skin and mucous membranes, often with scalloped edges, ranging in size from 1 to 4-5 cm or more. These ulcerative lesions are often preceded by bullous eruptions. Ulcerative lesions are rare and localized to the lower extremities, accompanied by pain that is aggravated by walking. Edges of the ulcers are firm, pinkish-blue in color, and elevated above the level of surrounding healthy skin. Base of the ulcers is covered with pale, granular tissue and a necrotic layer.
These eruptions are most commonly found on soles, especially in the interdigital spaces. Cases of involvement of trunk and perianal area have been reported. The eruptions leave scars.
This variant often coexists with more typical nail, mucosal, and cutaneous involvement, aiding in accurate diagnosis. Ulcerative lesions may progress to squamous cell carcinoma.Follicular lichen planus
Lichen planopilaris
Clinically, whitish atrophic or scarred patches may be observed on the scalp, which may be accompanied by complaints of increased hair loss, itching, scaling, burning, and tenderness of the scalp. These subjective symptoms may be exacerbated by exposure to ultraviolet light, scalp irritation, sweating, and stress.
Hair is easily removed from affected areas. Patches may be single or multiple and usually involve the crown and vertex of the scalp.
There are three subtypes of flat lichen: classic, frontal fibrosing alopecia, and Graham-Little-Piccardi-Lassueur syndrome.
The classic variant is characterized by patches of alopecia on the scalp and isolated typical patches on the trunk and extremities.
Frontal fibrosing alopecia presents with progressive scarring and hair loss from the frontal hairline and affects primarily middle-aged women.
Graham-Little-Piccardi-Lassueur syndrome is a triad of scarring alopecia of the scalp, widespread follicular papules on the trunk, and nonscarring hair loss in the axillary and pubic regions.
Clinical manifestations of this form of the disease typically develop unnoticed by patient, who may not seek medical attention until months or years after the onset of the disease.Palmoplantar lichen planus
Lichen planus localized on the palms and soles presents atypically. Diagnostic challenges arise in cases of isolated palmoplantar involvement. In these cases, skin thickening develops slowly with or without keratotic deposition resembling callus. Lesions are often localized on lateral areas of the hands and feet, and fingertips, although these are rarely involved.
These eruptions may also appear as small, flat or slightly sunken cornified areas, deeply located vesicles in dyshidrosis and, rarely, as bullous-ulcerative changes that may give rise to vegetative verrucous lesions.
In all these cases, single typical polygonal papular eruptions can be observed, which help in the correct diagnosis.
In rare cases, this form may be associated with areas of scarring alopecia on the hairy part of the scalp.Annular lichen planus
Linear and blaschkoid lichen planus
Usually seen in children, characterized by an arrangement of papules in stripes that may be linear, segmental, girdle-like, or following Blaschko's lines. The rash is localized to the trunk, extremities, and rarely face. Individual eruptions may appear as typical pruritic flat papules. Eruptions may also have a reticular, hyperkeratotic, or annular appearance.
Sometimes the cause of this form of the disease is the phenomenon of isomorphic reaction. Zosteriform localization of eruptions is possible, often as a result of previous herpetic infection.
Actinic lichen planus
Actinic lichen planus, also known as tropical lichen planus, is common in people from tropical regions (African, Middle Eastern, and Indian populations) and rare in Caucasians. Eruptions are more common in spring and summer, with improvement or remission during the winter months. Actinic form is observed in middle-aged patients, more often in women than in men. The exact pathogenesis is unknown, but sun exposure is clearly an important factor in the development of the disease. There are probably genetic, infectious, environmental or hormonal predisposing factors.
Clinically, it presents in three forms: annular, pigmented, and dyschromic.
The most common annular form is characterized by erythematous brownish annular plaques with or without atrophy. The pigmented form appears as hypermelanotic macules with a melasma-like appearance. The dyschromic form is the rarest and is characterized by appearance of whitish papules that often coalesce into pinhead-sized lesions.
The eruptions are localized on the face, particularly the forehead, cheeks and lips, upper chest, extensor surfaces of the forearms and dorsal surfaces of the hands. Actinic lichen planus is usually asymptomatic and may resemble actinic keratosis.Erythrodermic lichen planus
Erythrodermic form is characterized by sudden erythema of trunk and extremities with elevated temperature, edema, and the appearance of typical lichenoid papular eruptions. Atypical clinical presentation is due either to drug sensitization leading to drug eruption or to a combined course of lupus erythematosus and actinic lichen planus in the axillary and pubic areas. Cases have been reported in which erythroderma developed after extensive needling, sunbathing, and radiation therapy. Classic form of lichen planus may also progress to the erythrodermic stage.
This stage is characterized by diffuse, infiltrated reddish-purple plaques on the trunk, face, and extremities, accompanied by swelling and desquamation, masking the appearance of typical purplish papules, which may be found in small numbers after the process has subsided. In addition to erythroderma, typical elements of lichen planus, bullae and erosions may be observed. The eruptions are accompanied by intense pruritus.Hypopigmented lichen planus
Eruptive lichen planus
Perforating lichen planus
Nail lichen planus
Nail lichen planus occurs in 10-15% of patients and involves nail plate. It presents as an onychodystrophy with circulatory disorders (dryness, longitudinal ridges, pterygium, complete destruction of the nail plate). Characteristic changes typically develop simultaneously in several nails. In some patients, nail changes precede skin rashes and may even be the only manifestation of this dermatosis, in which case the diagnosis should be confirmed by histopathologic examination.
A classic symptom is the development of a pterygium, in which eponychium grows anteriorly and adheres to proximal part of the nail. This leads to fissuring of the nail and sometimes complete loss of the nail plate.
Another common symptom is trachyonychia, characterized by roughness of the nail plate, loss of transparency, and a grayish appearance.
Less common symptoms include onychoschizia (thinning, appearance of longitudinal lines, and distal splitting of the nail plate), onycholysis, longitudinal ridges (onychorrhexis), subungual hyperkeratosis, and complete disappearance of the nail plate (anonychia), which is seen in the erosive-ulcerative form.Inverse lichen planus
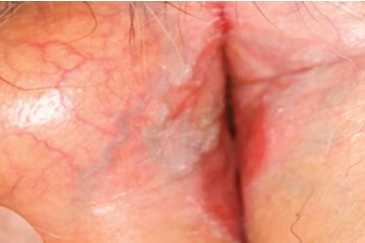
Inverse lichen planus is a rare clinical presentation characterized by discrete reddish-brown macules and papules. These eruptions are localized in the axillary folds, inguinal folds, inframammary folds. Koebner's phenomenon is characteristic.
Clinically, the eruptions have a localized erythematous character with blurred borders and areas of lichenification. Keratotic (horny) papules and erosions with complex contours may be present. Hyperpigmentation is also typical.Oral lichen planus
Oral lichen planus presents with small, grayish-white papules, up to 2-3 mm in diameter, located symmetrically on mucosa of both cheeks. These papules may coalesce to form a network of whitish reticular bands (Wickham's striae). Plaques with well-defined borders that protrude above the surrounding mucosa, resembling leukoplakia, may also occur (patchy form). When tongue is involved, white papules may be seen that coalesce into small plaques.
Subjective sensations are usually absent in typical form of oral lichen planus, but erosions or ulcers (especially in the elderly) may appear in the affected areas of the mouth, accompanied by a burning or painful sensation and discomfort with hot or cold water.
Hyperkeratotic oral lichen planus
Exudative oral lichen planus
Erosive-ulcerative oral lichen planus
Atrophic oral lichen planus
Bullous oral lichen planus
Atypical oral lichen planus
Penile lichen planus
Vulvar Lichen Planus
This form is relatively common. Lesions may be confined to the genitalia, coexist with oral mucosal involvement, or be part of a widespread process. Clinical manifestations in vulvar region may vary: they may present as the typical linear, reticular (white-gray lacy pattern), annular, or patchy forms of the disease. Alternatively, they may manifest as an erosive form associated with dystrophic changes, scarring, and disruption of normal vulvar anatomy.
A characteristic feature of the vulvovaginal variant is its chronic course with unexplained exacerbations, improvements, and remissions.Lichen Planus Pemphigoides
Lichen planus-lichen sclerosus overlap syndrome
Lichen planus-Lupus erythematosus overlap syndrome
Lichenoid drug eruption
Lichenoid drug eruptions may occur with oral administration, parenteral injection, and inhalation of drugs. The exact pathogenetic mechanism underlying the development of it is not fully understood. However, they are thought to be a direct effect of clones of autoreactive cytotoxic T cells directed against drug/antigen complexes recognized as foreign by keratinocytes and Langerhans cells.
Lichenoid eruptions typically occur several weeks or months after initiation of therapy. The nature of the eruption depends on drug dosage, patient response, re-exposure to the drug, and concomitant use of other medications. Drug-induced lichenoid eruptions are usually indistinguishable from classic lichen planus (multiple flat, pruritic, purplish papules) and tend to involve large areas of skin, even progressing to erythroderma.
Lesions are usually symmetrical on the trunk and limbs and, unlike lichen planus, do not involve body folds. They rarely occur on oral mucosa and lack the classic Wickham's striae. Persistent postinflammatory pigmentation is also characteristic, and sometimes alopecia and skin atrophy with anhidrosis due to sweat gland atrophy may occur.
Resolution of the rash is slow, typically within 1 to 4 months and sometimes up to 2 years. Occasionally, lichenoid drug eruptions may resolve spontaneously or periodically, even with continued use of the drug.Lichenoid contact dermatitis
Lichenoid reaction in graft-versus-host disease
In most cases, the diagnosis is based on clinical presentation. However, in cases where the patient has hypertrophic, atrophic, pigmented, vesicular, erosive-ulcerative, and follicular forms, typical elements for establishing a clinical diagnosis may be absent. To confirm the diagnosis, histological examination is performed.
Before initiating systemic treatment or deciding on further treatment approaches, laboratory tests are necessary:
- Complete blood count (CBC) and urinalysis.
- Blood biochemistry (ALT, AST, total bilirubin, triglycerides, cholesterol, total protein)
- Testing for the presence of antibodies to hepatitis C virus
- Urinalysis
Consultations with other specialists are recommended based on indications:
- Before initiating PUVA therapy, narrowband ultraviolet B phototherapy – consultations with an ophthalmologist, endocrinologist, general practitioner, and gynecologist to rule out contraindications
- Before prescribing antimalarial drugs to exclude contraindications, and during antimalarial drug therapy, ophthalmologist consultations are recommended every 1.5 to 3 months
- Consultation with a stomatologist may be recommended to determine the nature of isolated lesions of the oral mucosa
Differential diagnosis of classic lichen planus:
- Syphilis
- Atopic dermatitis
- Pityriasis rubra pilaris
- Darier disease
- Psoriasis
- Granuloma annulare
Differential diagnosis of eruptive lichen planus:
- Lichen nitidus
- Lichenoid Reactions
- Pityriasis lichenoides
- Sulzberger-Garbe Disease
- Keratosis lichenoides chronica
- Cutaneous tuberculosis
Differential diagnosis of bullous lichen planus:
- Lichen planus pemphigoides
- Dermatitis Herpetiformis
- Bullous Pemphigoid
Differential diagnosis of annular lichen planus:
- Granuloma Annulare
- Porokeratosis
- Tinea corporis
- Secondary Syphilis
- Superficial Basal Cell Carcinoma
Differential diagnosis of actinic lichen planus:
- Polymorphic Light Eruption
- Melasma
- Solar Lichenoid Reactions
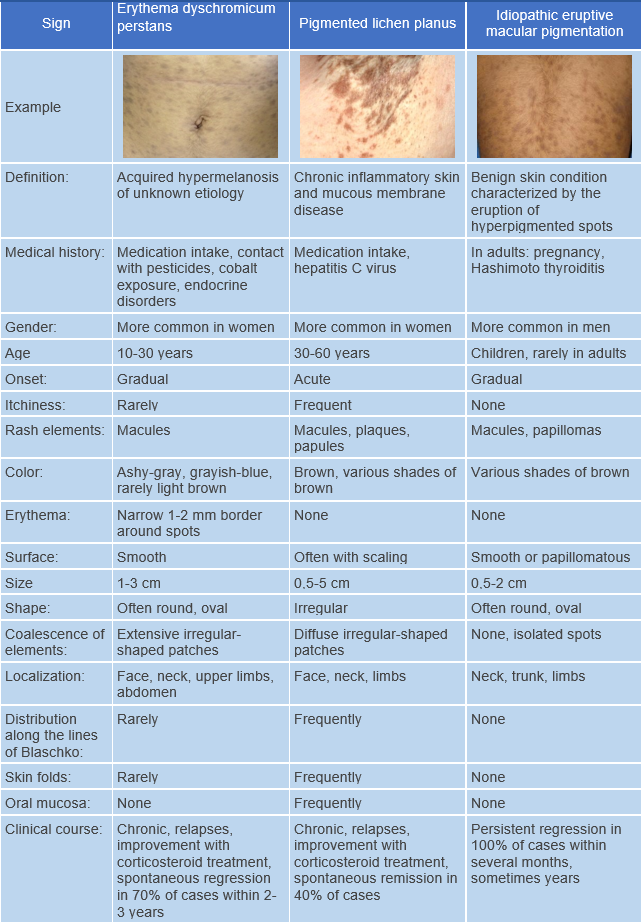
- Erythema dyschromicum perstans
Differential diagnosis of atrophic lichen planus:
- Lichen sclerosus
- Morphea
- Porokeratosis
Differential diagnosis of pigmented lichen planus:
- Erythema dyschromicum perstans
- Addison's Disease
- Melasma
Differential diagnosis of hypertrophic lichen planus:
- Lichen simplex chronicus
- Lichen amyloidosis
- Nodular prurigo
- Hypertrophic discoid lupus erythematosus
- Tuberculosis verrucosa cutis
Differential diagnosis of palmoplantar lichen planus:
- Palmoplantar Psoriasis
- Warts
- Callus
Differential diagnosis of linear lichen planus:
- Linear Psoriasis
- Lichen striatus
- Epidermal Nevus
- Linear morphea
Differential diagnosis of follicular lichen planus:
- Keratosis pilaris
- Lichen spinulosus
- Pseudopelade of Brocq
- Discoid Lupus Erythematosus
- Papular sarcoidosis
- Morphea
Differential diagnosis of nail lichen planus:
- Psoriasis
- Onychomycosis
- Lichen striatus
- Trachyonychia
- Alopecia areata
Differential diagnosis of oral lichen planus:
- Leukoplakia
- Candidiasis
- Nicotine Stomatitis
- Pemphigus vulgaris
- Lichenoid Reactions
- Discoid Lupus Erythematosus
- Addison's Disease
Differential diagnosis of penile lichen planus:
- Papular syphilis
- Candidal Balanitis
- Psoriasis
- Zoon's plasma cell balanitis
- Lichen sclerosus
- Bowenoid papulosis
- Circinate Balanitis(Reiter’s disease)
Differential diagnosis of vulvar lichen planus:
- Lichen sclerosus
- Psoriasis
- Lichen simplex chronicus
- Cicatricial Pemphigoid
- Plasma Cell Vulvitis
General Remarks on Therapy
- The choice of treatment method depends on the severity and localization of clinical manifestations, the form and duration of the disease, and information about the effectiveness of previous therapy.
- Treatment is not necessary if the oral mucosa is affected by reticular lesions of typical form without subjective sensations. In other cases, treatment is necessary.
Topical treatment
For limited eruptions, treatment starts with the use of medium to high-potency topical glucocorticosteroid preparations (alternating their use is possible):
- Betamethasone cream or ointment applied to the affected areas twice a day for 12 weeks or
- Clobetasol cream or ointment applied to the affected areas twice a day for 4-8 weeks or
- Fluocinolone acetonide cream, gel, or ointment applied to the affected areas twice a day for 4-8 weeks or
- Hydrocortisone-17 butyrate cream or ointment applied to the affected areas twice a day for 4-8 weeks or
- Triamcinolone ointment applied to the affected areas twice a day for 4-8 weeks or
- Mometasone cream, ointment, or lotion applied to the affected areas once or twice a day for 4-8 weeks or
- Betamethasone + salicylic acid ointment applied to the affected areas twice a day for 4-8 weeks or
Alternative Treatment Methods
- Tacrolimus ointment applied twice a day for 3 months.
- Calcipotriol ointment applied twice a day for 3 months.
Systemic Therapy
For patients with lichen planus, antimalarial drugs can be used as systemic therapy and can be combined with glucocorticosteroid preparations:
- Hydroxychloroquine 200 mg orally twice a day for 5 days, followed by a 2-day break; repeat treatment courses for 1-2 months or
- Chloroquine 250 mg orally twice a day for 5 days, followed by a 2-day break; repeat treatment courses for 1-2 months.
Systemic glucocorticosteroid preparations:
- Prednisolone 20-30 mg per day orally for 1-2 months with subsequent gradual tapering
To alleviate itching, one of the first-generation antihistamines is prescribed:
- Mebhydrolin 100 mg orally 2-3 times a day for 7-10 days or
- Clemastine 1 mg orally or intramuscularly 2-3 times a day for 7-10 days.
Additionally, to reduce itching:
- Hydroxyzine 25-100 mg per day orally for 28 days.
Non-pharmacological Treatment
For mild infiltration of the affected areas, narrow band medium wave phototherapy with a wavelength of 311 nm is administered 3-4 times a week for 6-12 weeks.
Patients with more pronounced infiltration of the affected areas may receive PUVA therapy with oral or topical application of a photosensitizer:
PUVA therapy with oral photosensitizer: Methoxsalen 0.6 mg per kg body weight or PUVA therapy with topical application of photosensitizer: Methoxsalen 0.5-1 mg/l for a course of 8 to 23 sessions
Treatment of Oral Lichen Planus
First-line treatments for oral mucosal lichen planus include topical glucocorticosteroid preparations:
- Betamethasone cream or ointment applied to the affected areas twice a day for 8 weeks or
- Triamcinolone ointment applied to the affected areas three times a day for 12 weeks or
- Fluocinolone acetonide cream, gel, or ointment applied to the affected areas twice a day for 4-12 weeks or
Additional pain-relieving and wound-healing agents are used:
- Aloe vera leaf liniment applied externally to the affected areas twice a day.
- Lidocaine + chamomile gel: A 0.5 cm strip is applied to painful or inflamed areas of the oral mucosa and gently massaged three times a day.
- Choline salicylate + cetylpyridinium chloride dental gel: Adults use 1 cm, and children use 0.5 cm of gel applied to the affected area of the oral mucosa 2-3 times a day before or after meals and before sleep.