Necrobiosis lipoidica is a chronic granulomatous disorder. It most commonly affects skin on the anterior surface of the shins, and a typical pattern is observed in association with diabetes (necrobiosis lipoidica diabeticorum). ICD-10 code: L92.1.
Necrobiosis Lipoidica is a rare complication of diabetes, often associated with severity of diabetic microangiopathy. It is observed in 0.3% of diabetic patients or 2% considering only type 1 diabetes cases. For patients without diabetes, the etiology of the condition is unknown.
Necrobiosis lipoidica not associated with metabolic disorders is typically described as granuloma annulare of Miescher. It also occurs primarily on the shins, but may spread to other parts of the body, particularly the face and hairy scalp, in the form of spotty or annular lesions.
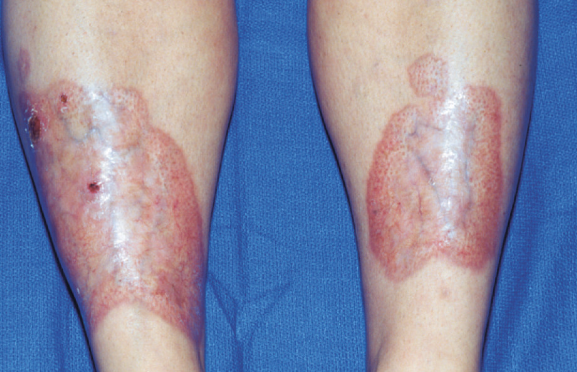
Necrobiosis lipoidica typically begins with bilateral nodular lesions on the shins. The nodules flatten and develop into oval plaques over several years and decades. In more advanced forms, the disease presents as single or multiple scleroatrophic plaques ranging in size from 5 to 15 cm. Chronic and painful ulcers may occur, especially in diabetic patients. In rare cases, persistent verrucous or ulcerated lesions may progress to carcinoma.
Lesions may also occur elsewhere, such as on the ankles, feet, upper extremities, and even on the face and hairy scalp, where they assume a ring shape and are often associated with scarring alopecia.- Diabetic dermopathy
- Granuloma Annulare
- Sarcoidosis
- Miescher's granuloma
- Actinic granuloma
- Stasis dermatitis
- Morphea
The prevalence of diabetic necrobiosis lipoidica has decreased significantly. This is probably due to the preventive effect of improved medical care for young and insulin-dependent patients. On the other hand, the specific treatment of diabetes does not influence the already existing necrobiosis lipoidica. This paradox characterizes this condition as a very specific complication of diabetes, which cannot be influenced only by the control of diabetic glycemia. However, it should be emphasized that strict control of diabetes, even if it does not improve the clinical picture of the disease, provides a better prognosis and reduces the risk of complications. In patients without diabetes, spontaneous remission may occur independent of any treatment
Topical treatment
Topical corticosteroids are medications that have some effect on this condition. Occlusive dressings or intralesional injections can reduce inflammation at the periphery and halt the progression of scleroatrophic plaques. However, they do not affect the scar changes at the center of the lesion, and patients often do not agree with the physician's opinion that the lesion has improved.
The drugs of choice in this case are high-potency corticosteroids: clobetasol propionate or betamethasone dipropionate 0.05% in gel or cream are applied for 3-4 weeks. Results are better in the early stages than in fully developed atrophic lesions. In cases of ulceration, some improvement can be achieved with the use of 20% benzoyl peroxide preparations and dressings containing hydrocolloid gels or bovine collagen.
Topical tretinoin has shown some success in some patients.
In some patients, topical psoralen and ultraviolet A (PUVA) therapy 1-2 times per week has been effective, even in cases of ulcerated lesions and regardless of diabetes association. After topical application of 0.15% methoxypsoralen emulsion, lesions are exposed to UVA at an initial dose of 0.5 J/cm², increasing by 20% with each subsequent session if the treatment is well tolerated. Complete clearance or significant improvement can be expected with a median cumulative UVA dose of less than 100 J/cm² if the lesions are not too atrophic.
Systemic Treatment
The list of drugs for which there have been reports of efficacy in short case studies is quite long:
- Aspirin 40-300 mg/day
- Clofazimine 200 mg/day
- Cyclosporine A 3-5 mg/kg per day
- Dipyridamole 300 mg/day
- Heparin
- Methylprednisone
- Mycophenolate mofetil
- Nicotinamide 1.5 g/day
- Pentoxifylline 800-1200 mg/day
- Prostaglandin E1 4 mg intravenously twice a day
- Ticlopidine 500 mg/day
These drugs were selected from antithrombotic, vasodilator, anticoagulant, anti-inflammatory, and even immunosuppressive agents such as cyclosporine A and mycophenolate mofetil. Patients receiving cyclosporine A (3-4 mg/kg per day for 3-4 months) showed significant improvement in clinical presentation, with relapses observed after discontinuation of the drug.
Only aspirin has been tested in controlled trials, but it showed no effect, even in combination with dipyridamole, compared with placebo.
Good results have been attributed to systemic steroids with strict glycemic control. In a series of 6 patients treated with methylprednisolone (1 mg/kg per day for 1 week, then 40 mg/day for 4 weeks with gradual tapering over the following 2 weeks), the peripheral granulomatous areas completely resolved in all patients, leaving only central atrophic area with a waxy yellowish appearance. There were no relapses during a 7-month follow-up, and the lesions remained stable in size and appearance. Similar results have been reported in case reports.
Surgical treatment
Surgical removal of the painful ulcerated necrobiosis is proposed, followed by application of split grafts or tissue engineered dermal grafts. The lesion is replaced by a larger scar attached to the underlying muscle and bone. There is a risk of recurrence of necrobiosis lipoidica around the scar, which should be explained to the patient. Surgical treatment is avoided with arterial insufficiency or if the patient is concerned about cosmetic results.
If a 6-week regimen of systemic corticosteroids (prednisone at an initial dose of 1 mg/kg, gradually tapered) with strict glycemic control in diabetic patients fails, surgical treatment may be offered. For severe ulcerated necrobiosis lipoidica, patient may be offered local PUVA therapy or systemic treatment with cyclosporine A prior to surgical treatment.