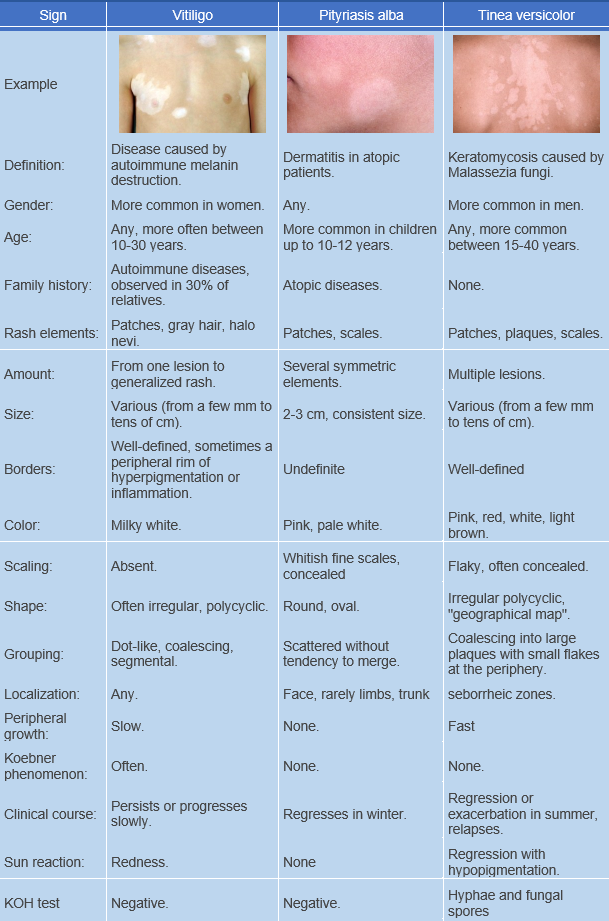
Pityriasis alba is a mild eczematous childhood dermatitis characterized by multiple, occasionally solitary, hypopigmented patches with indistinct borders. ICD-10 code: L30.5.
It is a common condition in children and adolescents, most often occurring between the ages of 3 and 16 (with 90% of cases occurring before the age of 12), and very rarely seen in adults. The highest number of cases is observed in children with atopic dermatitis, suggesting it could be considered a symptom of this condition.
The pathogenesis is unclear. Currently, it's believed that pityriasis alba is a mild eczematous dermatitis with subsequent hypopigmentation due to impared melanosome transfer from melanocytes to keratinocytes. Some theories suggest it's a post-inflammatory hypopigmentation in atopic children.
Several studies have suggested possible roles in the pathogenesis of the disease, including pityrosporin, a substance produced by Malassezia yeast that prevents UV exposure, iron deficiency anemia, copper deficiency, and the presence of atrophic sebaceous glands leading to skin xerosis.
Other researchers consider pityriasis alba to be an abortive form of bacterial skin infection caused by Streptococcus.
Peak incidence occurs in spring. Predisposing factors include warmth, humidity, detergents, soaps, frictional clothing, chemicals and stress.The disease begins with the appearance of pink round or oval spots 0.5 to 3 cm in diameter (erythematous stage), which fade over several weeks and turn into white spots with indistinct borders (hypopigmented stage). Due to the mild nature of the clinical manifestations of the erythematous stage, it often goes unnoticed by patients and/or their parents.
Preferred sites include face (especially the cheeks), shoulders, and arms. In rarer cases, it may appear on the neck and trunk. A widespread rash has been described in infants and young adult females 18-25 years old (generalized pityriasis alba). Lesions are typically multiple, but solitary spots can also occur.
A characteristic feature is the absence of a tendency for the elements to fuse. Mild pruritus is occasionally noted. A characteristic symptom is the appearance of occult scaling, which increases when the lesion is scraped. The spots may persist from a few weeks to several years and then regress spontaneously.Diagnosis is based on clinical data. In some cases, testing for fungi (KOH test) may be necessary.
Wood's lamp examination helps identify barely visible spots and differentiate the condition from vitiligo.Emollients, sunscreen, 1% hydrocortisone cream or ointment applied once daily for up to 10 days
There are reports of effective use of topical preparations containing calcipotriol and tacrolimus.
Creams containing antibiotics may be used:
Erythromycin ointment applied twice daily for 7-14 days.
Fusidic acid cream or ointment (2%) applied externally to the affected area 3 times daily for 7-14 days.
Mupirocin ointment (2%) applied externally to the affected area 2-3 times a day for 7-14 days.
Prognosis is favorable; post-inflammatory hypopigmentation may persist for up to one month after treatment.