Cutaneous melanoma is a malignant neoplasm of neuroectodermal origin that arises from melanocytes (skin pigment cells). ICD-10 Code: C43.
There is no single etiological factor for the development of melanoma. The most important risk factor for sporadic (non-inherited) forms of cutaneous melanoma is considered to be exposure to ultraviolet radiation, both type B (wavelength 290 - 320 nm) and type A (wavelength 320 - 400 nm). Skin sensitivity to ultraviolet radiation varies from person to person and can be classified into 6 types, with types 1 and 2 being the most sensitive (and therefore most likely to cause sunburn) and types 5 and 6 being the least sensitive. Other risk factors include the presence of more than 10 dysplastic nevi, more than 100 common acquired nevi, red hair (typically associated with phototype 1 skin), intense and regularly repeated sun exposure during childhood, and the presence of giant moles, as well as the presence of giant or congenital nevi (covering more than 5% of the body surface area), a family history of cutaneous melanoma, a personal history of cutaneous melanoma, dysplastic nevus syndrome, use of PUVA therapy (for psoriasis), xeroderma pigmentosum, congenital or acquired immunodeficiency (e.g. g., organ transplantation or other conditions requiring immunosuppressive therapy). Risk factors for melanoma at other sites are not well understood.
Classification:
- Superficial spreading melanoma
- Lentigo melanoma
- Nodular melanoma
- Subungual melanoma
- Acral melanoma
Superficial spreading melanoma
The most common malignant tumor of melanocytic origin in the white population, characterized by its early-stage development, spreading along the surface of the skin. Superficially spreading melanoma accounts for 70% of melanoma cases among the white population and 60% of all melanoma types. The disease typically occurs between the ages of 30 and 50 and is more common in women.
On apparently unchanged skin, a spot (or a flat papule) appears with a diameter of 2-3 mm, gradually increases in size. The affected area becomes oval or irregular in shape, often with one or more depressions. Gradually, thickening occurs, forming an asymmetrical plaque with clear borders, evenly raised above the surface of the skin. The average diameter is 8-12 mm, with early formations ranging from 5 to 8 mm and more advanced ones from 10 to 25 mm.
As the tumor grows, the surface of the affected area becomes uneven, bumpy, crusted, easily injured, bleeding, and nodules may develop. The coloration includes a combination of brown, dark brown, blue, black and red colors, with areas of regression appearing gray or bluish gray.
It can occur anywhere on the body. The most common site is the upper back in both men and women, with the shin area in women and the front of the thighs and torso in men. The tumor takes 1-2 years to develop.
Lentigo Melanoma (Lentigo Maligna Melanoma)
It occurs in about half of cases in people over the age of 65 and is most common in European people with skin types I, II, and III. It accounts for 5-10% of all cutaneous melanoma cases.
Lentigo maligna, which serves as a precursor to lentigo melanoma, initially appears as a single, flat spot with uneven color in various shades of brown and black. The appearance of papules or nodules on the surface of the spot indicates the invasion of tumor cells into the dermis and the progression of the condition to the next stage - lentigo melanoma. This process can take several years, sometimes up to 10-20 years.
The affected area takes on an irregular shape, resembling a geographic map with "peninsulas" with irregular borders ranging in size from 3 to 20 cm or more. Papules or nodules of dark brown, black, and sometimes pinkish or white-gray regression areas are observed on the surface of the flat spot, along with blue patches (accumulations of melanocytes in the dermis).
This new growth is most commonly found on exposed areas of the skin such as the face, neck, forearms, backs of the hands, and shins.Nodular Melanoma
Nodular melanoma accounts for about 14 to 20% of all melanoma cases. It primarily affects Europeans in middle age. Development of the tumor on clear skin or from a pigmented nevus takes between 6 and 18 months.
Nodular melanoma begins its development immediately with the vertical growth phase. The tumor is uniformly elevated above the skin surface and appears as a thick plaque. In cases of exophytic growth, it forms a protruding round nodule resembling a "blueberry" or a polyp. Typically, the color is uniform, dark blue or bluish black, although polypoid growths can sometimes be pink (non-pigmented) with a brownish coating.
In early stages, the affected area measures 1-3 cm, but it can grow over time. The melanoma has a regular, oval, or circular shape with clear borders. Over time, surface of the tumor may become ulcerated and covered with a bloody crust. Black nodules (metastatic foci) often appear around the melanoma.
It is most often found on parts of the body that are relatively less exposed to sunlight. In women, it is often found on the shins.Acral Melanoma
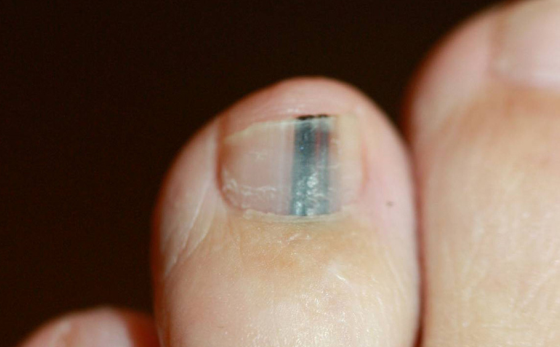
Subungual Melanoma
Subungual melanoma occurs in the nail bed and develops from the nail matrix. It is found in people between the ages of 20 and 80 (with an average age of 55). It accounts for approximately 2.5 to 3.5% of skin melanomas.
Fingers are twice as likely to be affected as toes, with the thumb involved in 80% of cases, possibly due to increased susceptibility to trauma and exposure to ultraviolet radiation. On the soles, subungual melanoma is also predominantly localized on the thumb, less frequently on the II and III digits.
It is characterized by a subungual spot or longitudinal brown or dark-blue stripes associated with pigmentation of the cuticle. Gradually, the nail plate in the pigmented area deteriorates and separates. In its place there is rapid growth of granulations, sometimes mushroom-shaped, bluish-black in color, with infiltration of the underlying and surrounding tissues. A pathognomonic sign associated with the late stage of melanoma is Hutchinson's sign (pigmentation in the area of the posterior eponychium).
The course of melanoma on the toes is generally less aggressive than on the fingers.Oral Melanoma
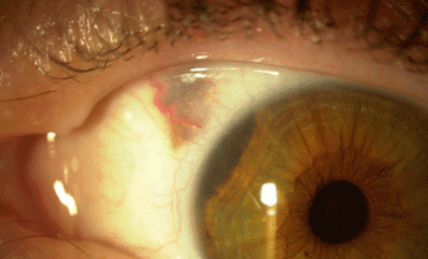
Ocular Melanoma
Penile Melanoma
Vulvar Melanoma
Anorectal Melanoma
Amelanotic Melanoma
Desmoplastic Melanoma
Neurotropic Melanoma
Childhood Melanoma
Childhood melanoma is categorized into infantile melanoma (from birth to one year of age), childhood melanoma (from one year to the onset of puberty), and adolescent melanoma (from 13 to 16 years of age).
In 50-92% of cases, childhood melanoma develops at the site of congenital giant melanocytic nevi during the first five years of life, with an estimated lifetime risk of developing melanoma of 6-7%.
In healthy skin, melanoma in children practically does not develop. In some cases, tumors may develop in children with dysplastic melanocytic nevi, a family history of melanoma, pigmentary xeroderma, or after immunosuppression. Familial cases account for approximately 10% of cases and tend to develop at an earlier age. Intense exposure to ultraviolet radiation plays a significant role in the development of melanoma.
Childhood melanoma is rare, accounting for 0.3% of cases in children with other malignancies. It is most commonly observed in children between the ages of 4-6 and 11-15 years. The male to female ratio is approximately 1:1.5.
Melanomas that develop before the age of 16 are most common on the trunk (50%), followed by the lower extremities (20%), head and neck (15%), and upper extremities (15%). Their size can vary from 0.5 to 7 cm or more, especially in melanomas growing from giant pigmented nevi. The appearance of these neoplasms is variable. In 95% of cases, melanomas have a broad base, with colors ranging from black to normal skin tone.Congenital Melanoma
Spitzoid Melanoma
Nevoid Melanoma
Polypoid Melanoma
Metastatic Melanoma
It is recommended that the patient's complaints and medical history be obtained in order to identify factors that may influence the choice of treatment tactics, diagnostic methods, and secondary prevention. When a patient first presents with complaints of pigmented skin lesions, it is strongly recommended to expand the area of examination and assess the condition of all skin surfaces (including the hairy part of the head and feet). Primary multiple synchronous tumors (melanoma and non-melanoma skin tumors) are found in 5-10% of patients.
The ABCDE of melanoma:
- Asymmetry
- Border irregularity
- Color variations (2 or more shades)
- Diameter more than 6 mm
- Evolving
7-Point Melanoma Recognition System (7PCL):
- Change in size
- Change in shape
- Change in color
- Inflammation
- Crusting or bleeding
- Sensory change
- Diameter more than 6 mm
Laboratory Tests:
Pending morphologic confirmation of the diagnosis, laboratory diagnosis is not recommended unless concomitant pathology or the patient's general condition makes it necessary for the safe performance of a biopsy. After confirmation of the diagnosis, complete blood count and blood biochemistry (including lactate dehydrogenase level) and tumor marker S100b could be recommended.
Biopsy:
An excisional biopsy of the suspicious pigmented lesion with a margin of no more than 5 mm (an acceptable margin is 1-3 mm) may be used to confirm the diagnosis and guide further evaluation and treatment plans.
It is recommended that skin incisions be made in the direction of the nearest lymph collector, parallel to the lymphatic vessels of the skin (rather than following skin lines or natural folds), so that scar revision (if necessary) can be performed without difficulty.
Excisional biopsy of a suspicious flat pigmented skin lesion can be safely performed under local infiltrative anesthesia. It is advisable to avoid damaging the lesion to be removed until it is excised.
If the diagnosis of cutaneous melanoma is confirmed, the scar is excised with a wide margin within 4-8 weeks after biopsy, depending on the histologic characteristics of the tumor.Superficial Spreading Melanoma:
- Melanocytic nevus
- Atypical (dysplastic) nevi
- Seborrheic keratosis
- Solar lentigo
Lentigo Melanoma:
- Pigmented actinic keratosis
- Bowen's disease
- Seborrheic keratosis
- Solar lentigo
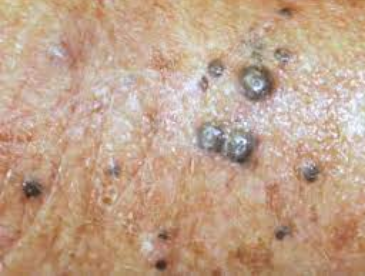
Nodular Melanoma:
- Melanocytic nevus
- Spitz nevus
- Seborrheic keratosis
- Hemangioma
- Pyogenic granuloma
- Kaposi Sarcoma
- Angiokeratoma
- Pigmented basal cell carcinoma
- Blue nevus
- Dermatofibroma
Subungual Melanoma:
- Longitudinal melanonychia
- Melanocytic nevus
- Pyogenic granuloma
- Subungual hematoma
Acral Melanoma:
- Plantar wart
- Talon noir
- Acral nevus
Desmoplastic Melanoma:
- Malignant Schwannoma (anaplastic neurilemmoma)
- Blue nevus
- Dermatofibroma
- Neurofibroma
- Scar
- Spitz nevus